When a patient gets sick after taking a new medication, how do you know if the drug actually caused the problem? It’s not always obvious. Maybe it was the infection they already had. Or the other meds they’re on. Or just bad luck. That’s where the Naranjo Scale comes in. It’s not magic. It’s not a lab test. It’s a simple, 10-question checklist that helps doctors, pharmacists, and nurses figure out if a side effect is really linked to a drug-or if something else is to blame.
Why the Naranjo Scale Still Matters Today
The Naranjo Scale was created back in 1981 by a team of researchers in Canada. They were trying to fix a big problem: too many adverse drug reactions (ADRs) were being misreported. Some were blamed on drugs when they weren’t. Others were ignored because no one could prove the link. The thalidomide disaster in the 1960s had shown how deadly that could be. So they built a tool that didn’t rely on guesswork. Today, over 40 years later, it’s still the most-used tool in hospitals and drug safety centers around the world. Why? Because it works. It turns a messy, confusing situation into a clear, step-by-step process. You don’t need fancy equipment. Just a pen, a form, and some basic knowledge of the patient’s history. In 2023, a study in Cureus showed that hospitals using the Naranjo Scale reduced errors in ADR reporting by nearly 70%. That’s not just paperwork-it’s saving lives. When you know for sure a drug caused a reaction, you can stop giving it. You can warn other patients. You can avoid another tragedy.How the Naranjo Scale Actually Works
The scale has 10 questions. Each one gets a score: -1, 0, +1, or +2. You answer based on what you know-yes, no, or don’t know. Then you add up the points. The total tells you how likely the drug caused the reaction. Here’s what each question looks like, in plain language:- Has this reaction been reported before with this drug? (+1 if yes)
- Did the reaction happen after the drug was given? (+2 if timing fits, -1 if it didn’t)
- Did the patient get better after stopping the drug? (+1 if yes)
- Did the reaction come back when the drug was given again? (+2 if yes, -1 if it got worse)
- Could something else have caused it? (-1 if yes, +2 if no)
- Did giving a placebo cause the same reaction? (-1 if yes, +1 if no)
- Was the drug at a toxic level in the body? (+1 if yes)
- Did the reaction get worse when the dose went up? (+1 if yes)
- Has the patient had this reaction to the same drug before? (+1 if yes)
- Is there lab or test evidence confirming the reaction? (+1 if yes)
That’s it. Ten questions. No blood tests. No scans. Just facts you already have.
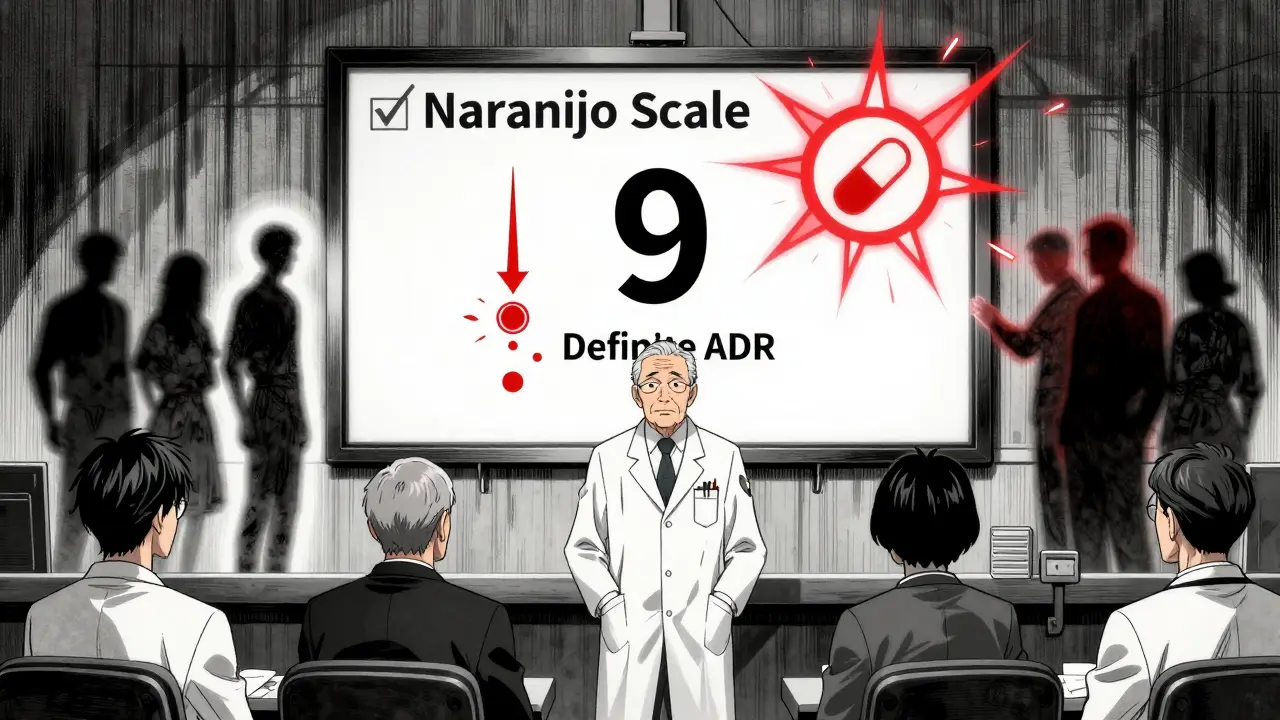
What the Scores Mean
Once you add up the points, you get one of four results:- 9 or higher = Definite ADR. The drug almost certainly caused it. You’ve got strong timing, improvement after stopping, and no other likely cause.
- 5 to 8 = Probable ADR. Very likely, but maybe not 100%. The reaction fits, it got better after stopping, but you couldn’t test it again or there’s a small chance something else was involved.
- 1 to 4 = Possible ADR. The timing lines up, but there are other explanations. Maybe the patient had a virus, or another drug could’ve done it. You can’t rule it out, but you can’t confirm it either.
- 0 or lower = Doubtful. The reaction probably wasn’t caused by the drug. Maybe it was the illness, stress, or another factor entirely.
These categories aren’t just labels. They drive real decisions. A ‘definite’ ADR gets reported to drug safety agencies. A ‘probable’ one triggers a review in the hospital. A ‘possible’ one gets documented for future reference. A ‘doubtful’ one? You move on.
Where the Naranjo Scale Falls Short
It’s not perfect. And it never claimed to be. One big problem? Rechallenge. Question 4 asks: “Did the reaction come back when the drug was given again?” Sounds logical. But if the reaction was severe-like liver failure or a dangerous rash-no doctor would ever give that drug back. So you answer “don’t know.” That knocks off 2 points. Suddenly, a definite reaction becomes probable. Or worse. Question 6 is even trickier. It asks about placebo testing. In theory, you’d give the patient a sugar pill to see if the reaction still happens. But that’s unethical today. You can’t risk harming someone just to prove a point. So most clinicians skip it-or answer “no” by default. That’s not accurate. It’s just safe. Another issue? Polypharmacy. Most patients, especially older ones, take five, six, or more drugs. The Naranjo Scale only looks at one drug at a time. If three drugs could’ve caused the reaction, the scale doesn’t help you pick which one. That’s why tools like the Liverpool Scale were developed-but they’re not as widely used. And then there’s the rise of new medicines. Biologics. Immunotherapies. Gene therapies. These drugs don’t work like old-school pills. Their side effects can show up weeks later. Or last forever. The Naranjo Scale wasn’t built for that. It’s designed for reactions that happen within hours or days. That’s a growing gap.How Professionals Use It Today
In real hospitals, the Naranjo Scale isn’t just a paper form anymore. Many places use digital versions built into their electronic health records. Epic, Cerner, and other systems now auto-fill some of the questions-like whether the drug was given before the reaction, or if the patient’s liver enzymes spiked. A 2023 study showed that using a digital Naranjo calculator cut assessment time from 11 minutes to under 5. Error rates dropped from 28% to just 9%. That’s huge. Nurses and pharmacists who used to dread filling out the form now do it in seconds. On Reddit, pharmacists say they use it daily. One wrote: “It forces us to think, not just assume.” Another said: “I used to think every rash was an allergy. Now I ask: Did it start after the new antibiotic? Did it go away when we stopped it? That’s the Naranjo Scale in action.” But it’s not just for hospitals. Drug companies use it to evaluate reports from patients. Regulators like the FDA and EMA require structured causality assessments-and the Naranjo Scale is the default tool. If you’re reporting a serious side effect, you’re likely using this scale.
What You Should Know If You’re a Patient
You probably won’t fill out the Naranjo Scale yourself. But you can use it to ask better questions. If you had a reaction after starting a new drug, ask your doctor: “Could this be caused by the medication? How do we know?” Then ask: “Was it checked using a standard tool?” If they say yes, ask what the score was. If they don’t know, that’s a red flag. You can also track your own symptoms. Note when you started the drug. When the side effect began. Did it get better after you stopped? Did it come back if you restarted? That’s the Naranjo Scale in your hands. It’s not about blaming the drug. It’s about understanding what’s really happening in your body.What’s Next for the Naranjo Scale?
The scale isn’t going away. But it’s changing. In 2024, the International Council for Harmonisation proposed replacing Question 6 (placebo) with a question about drug levels in the blood. That’s smarter. More ethical. More useful. Some researchers are building AI tools that combine the Naranjo Scale with real-time data-like lab results, genetic info, and other meds. These tools can suggest scores automatically, then let the clinician adjust. But the core idea stays the same: structure beats guesswork. Evidence beats intuition. Even as new drugs come out, the Naranjo Scale remains the foundation. It’s not the final answer. But it’s the first real question you should ask.Final Thoughts
The Naranjo Scale isn’t glamorous. It doesn’t make headlines. But every time a pharmacist catches a dangerous drug reaction before it harms another patient, that’s the scale at work. It’s simple. It’s old. It’s imperfect. But it’s the best tool we have for turning chaos into clarity. If you’re in healthcare, learn it. Practice it. Use it. If you’re a patient, understand it. Ask about it. Your safety depends on it.What is the Naranjo Scale used for?
The Naranjo Scale is used to determine whether an adverse drug reaction (ADR) is likely caused by a specific medication. It’s a 10-question tool that assigns points based on clinical evidence, helping healthcare professionals classify reactions as definite, probable, possible, or doubtful.
How accurate is the Naranjo Scale?
Studies show moderate accuracy, with inter-rater reliability scores (kappa) between 0.4 and 0.6. It’s more consistent than other tools like WHO-UMC, but accuracy depends on the clinician’s knowledge. Misjudging alternative causes or skipping rechallenge can skew results. Digital versions reduce errors by up to 70%.
Can the Naranjo Scale be used for any drug?
Yes, it works for any medication-antibiotics, painkillers, blood pressure drugs, even biologics. But it was designed for traditional small-molecule drugs. For newer therapies like immunotherapies, where reactions can appear months later, the scale’s timing rules may not fit well. It’s still used, but with caution.
Why is rechallenge sometimes skipped in the Naranjo Scale?
Rechallenge means giving the drug again to see if the reaction returns. It’s skipped because it’s dangerous. If a patient had a severe reaction-like anaphylaxis or liver failure-reintroducing the drug is unethical and risky. Most clinicians answer "don’t know," which lowers the score. This is a known limitation of the scale.
Is the Naranjo Scale still used in 2025?
Yes. As of 2025, it’s used in 78% of published ADR case reports and is the default tool in most hospital pharmacovigilance programs. Regulatory agencies like the FDA and EMA still accept it for formal reporting. Digital tools and AI are enhancing it, but the core scale remains unchanged because it’s simple, reliable, and validated over decades.
How do I learn to use the Naranjo Scale?
Start with the original 10 questions and practice on real cases. Many hospitals offer 2-4 hours of training. Free resources like Fiveable’s pharmacology module include 12 interactive case studies. Digital calculators on GitHub or built into EHR systems can help you learn by doing. Most people become proficient after 5-10 cases.




Janette Martens
December 28, 2025 AT 14:37Marie-Pierre Gonzalez
December 29, 2025 AT 16:11Louis Paré
December 30, 2025 AT 10:32Ryan Touhill
December 31, 2025 AT 05:45Teresa Marzo Lostalé
December 31, 2025 AT 11:03ANA MARIE VALENZUELA
January 1, 2026 AT 17:34Bradly Draper
January 2, 2026 AT 01:11Gran Badshah
January 2, 2026 AT 04:12Ellen-Cathryn Nash
January 3, 2026 AT 09:14Samantha Hobbs
January 4, 2026 AT 19:05Nicole Beasley
January 5, 2026 AT 04:29sonam gupta
January 6, 2026 AT 12:45Vu L
January 8, 2026 AT 06:23oluwarotimi w alaka
January 9, 2026 AT 07:23