Medication Metabolism Guide
This tool helps you understand how your genetic makeup might affect your response to certain medications. Based on the information in the article, some people may benefit from pharmacogenetic testing to avoid side effects or ineffective treatment.
Have you ever taken a medication that didn’t work-or made you feel worse? Maybe you were on an antidepressant for months with no improvement, or you got sick after a standard dose of a painkiller. You’re not alone. For many people, the problem isn’t the drug itself. It’s their genes.
What Is Pharmacogenetic Testing?
Pharmacogenetic testing looks at your DNA to see how your body processes medications. It checks specific genes that control enzymes responsible for breaking down drugs. The most common ones are CYP2D6, CYP2C19, DPYD, and SLCO1B1. These genes tell your body whether to metabolize a drug slowly, normally, or too fast.
Think of it like this: your liver is a factory. Some people’s factories run at full speed, others barely turn on. A drug that works perfectly for one person might build up to toxic levels in another-or get broken down before it can help. Testing finds out which kind of factory you have.
It’s not science fiction. The FDA tracks over 300 drug-gene interactions. For example, if you have a variant in the DPYD gene, giving you standard doses of the cancer drug 5-fluorouracil could cause life-threatening toxicity. But if you get tested first, doctors can cut your dose by half-and save your life.
Who Benefits the Most?
This isn’t for everyone. But for certain groups, the payoff is clear.
- People on antidepressants: About 25% of people don’t respond to SSRIs like sertraline or fluoxetine. Testing for CYP2D6 and CYP2C19 can show if you’re a slow metabolizer (risk of side effects) or a rapid one (drug won’t work). A 2022 JAMA study found testing reduced inappropriate prescriptions by 30% in patients with major depression.
- Heart patients on blood thinners: Warfarin dosing has always been a guessing game. But if you have variants in CYP2C9 or VKORC1, you might need just 1 mg per day instead of 5 mg. Too much? Risk of bleeding. Too little? Risk of stroke.
- Those on statins: If you’ve quit your cholesterol drug because of muscle pain, you might carry a variant in SLCO1B1. That variant makes statins more likely to build up in your muscles. Testing can help you switch to a safer alternative-without trial and error.
- Cancer patients: For drugs like 5-fluorouracil or tamoxifen, genetic testing isn’t optional-it’s standard in many clinics. One wrong dose can be fatal.
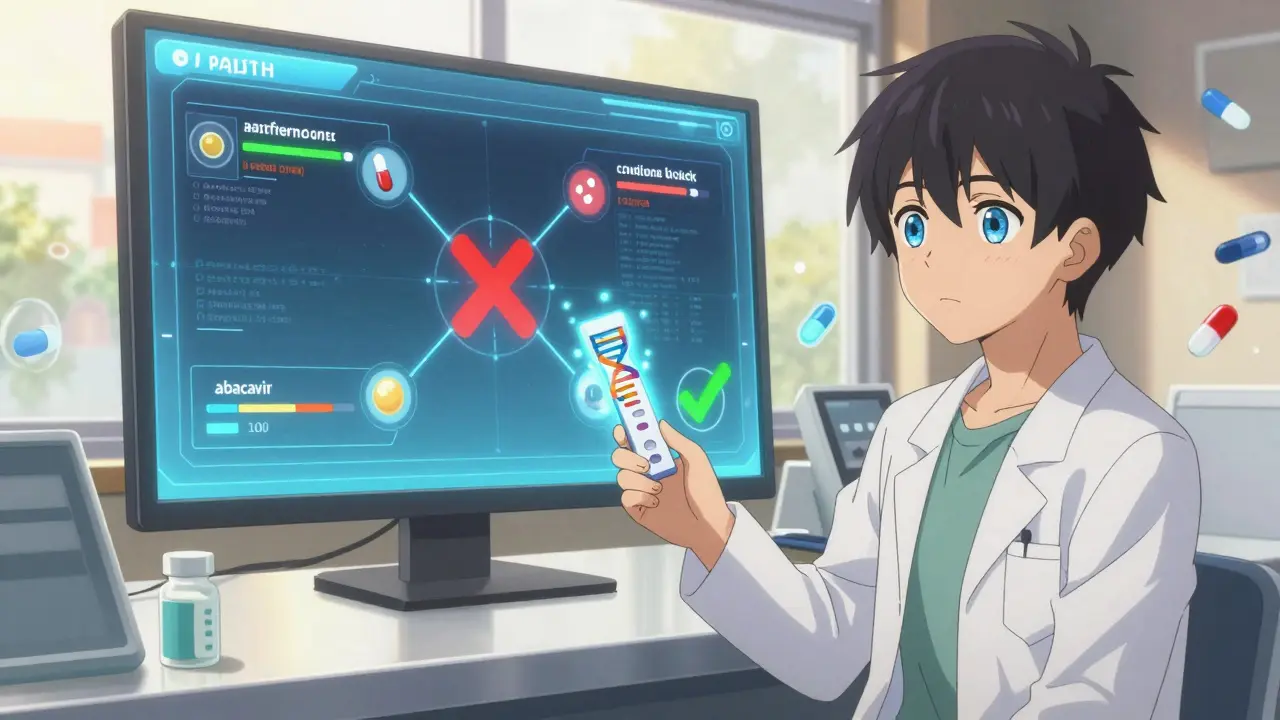
- People with HIV: Before starting abacavir, testing for HLA-B*57:01 is mandatory in most countries. Without it, 5-8% of people develop a deadly allergic reaction. With testing? That number drops to near zero.
These aren’t rare cases. About 1 in 4 people have at least one gene variant that affects how they respond to a common drug. And for those who’ve had bad reactions before, the odds are even higher.
How It Works
Getting tested is simple. You spit into a tube or get a cheek swab. No needles, no fasting. The sample goes to a lab, and in 7-14 days, you get a report.
Results don’t say ‘good’ or ‘bad.’ They say: poor metabolizer, intermediate, normal, rapid, or ultrarapid-for each gene tested. That tells your doctor how to adjust your dose or pick a different drug.
For example:
- Poor metabolizer of CYP2D6: Avoid codeine. Your body can’t turn it into morphine, so it won’t relieve pain. Instead, use acetaminophen or ibuprofen.
- Ultrarapid metabolizer of CYP2D6: Don’t take tramadol. You’ll turn it into morphine too fast-risking overdose.
- Intermediate metabolizer of CYP2C19: Clopidogrel (Plavix) won’t work well. Your doctor should switch you to prasugrel or ticagrelor.
These aren’t theoretical. Real patients have avoided hospitalizations, ER visits, and even death because of this info.
The Catch: It’s Not Perfect
Let’s be honest. This isn’t a magic bullet.
First, it only applies to about 300 of the 1,500+ drugs you might take. Most antibiotics, antivirals, and common painkillers aren’t covered yet.
Second, genes aren’t destiny. A 2023 study found that 41% of doctors misinterpret the results-especially if they’re not trained in pharmacogenetics. A ‘poor metabolizer’ label doesn’t always mean you can’t take the drug. Sometimes, lowering the dose works fine.
Third, some results are unclear. About 15-20% of tests show variants with unknown meaning. That’s frustrating. Your doctor might say, ‘We don’t know what this means.’
And then there’s cost. Out-of-pocket, a full panel runs $250-$500. Insurance might cover it if you’re on a high-risk drug like warfarin or abacavir-but rarely for general screening. In Australia, Medicare doesn’t yet fund it outside of specific cancer or HIV cases.
Finally, even with perfect results, your body still responds to age, diet, liver health, and other drugs you’re taking. Genetics is one piece of the puzzle-not the whole picture.
What the Evidence Really Shows
Is it worth it?
Let’s look at the data.
For abacavir and HLA-B*57:01: Testing prevents death. No debate.
For clopidogrel and CYP2C19: Poor metabolizers have a 50% higher risk of heart attack or stroke. Switching drugs saves lives.
For statins and SLCO1B1: Patients who got tested and switched drugs had 60% better adherence after three months. Those who didn’t? Only 33% stayed on their meds.
For antidepressants: Testing reduces bad prescriptions by 30%. But after 24 weeks, symptom improvement was only slightly better than usual care. So it helps avoid side effects-but doesn’t guarantee you’ll feel better.
Bottom line: It’s best for preventing harm, not always for boosting results.
Should You Get Tested?
Ask yourself these questions:
- Have you had a bad reaction to a medication-rash, nausea, dizziness, muscle pain, or no effect at all?
- Are you on a drug with known genetic links (antidepressants, blood thinners, statins, cancer meds)?
- Do you take multiple medications? (More drugs = more chance of bad interactions.)
- Is your doctor open to using genetic data? (If they say ‘we don’t use that,’ find one who does.)
If you answered yes to any of these, testing could be life-changing.
Start by talking to your doctor or pharmacist. Ask: ‘Is there a genetic test for the drug I’m taking?’ If they don’t know, ask for a referral to a clinical pharmacologist or a specialty pharmacy like Avant Pharmacy, which offers genetic counseling.
Don’t buy a direct-to-consumer test from a website unless you can get it interpreted by a professional. Many of these tests give confusing reports with no clinical guidance.
And if you’re healthy and just curious? Wait. The science is still catching up. You’re better off waiting until you’re prescribed a drug with a known genetic risk.
What’s Next?
Pharmacogenetics is growing fast. By 2030, the market will be over $21 billion. Hospitals like Mayo Clinic and Vanderbilt already have genetic data built into their electronic records. When you log in, the system flags: ‘Patient is a CYP2D6 poor metabolizer-avoid this drug.’
In Australia, adoption is slower. But with Medicare expanding coverage for genetic tests in oncology and mental health, it’s only a matter of time.
One thing’s certain: the era of ‘one-size-fits-all’ prescribing is ending. Your genes matter. Not because they’re magic-but because they’re real, measurable, and powerful.
If you’ve been frustrated by meds that didn’t work-or hurt you-this might be the missing piece. Not for everyone. But for enough people? It’s not just helpful. It’s essential.






Akriti Jain
January 21, 2026 AT 07:12So you're telling me my body just didn't like Zoloft because my DNA is a glitchy iPhone 5? 😏 I'm just glad I didn't take that warfarin after my yoga retreat. My grandma says my genes are cursed. I believe her. 🧬💀
Mike P
January 21, 2026 AT 09:20Look, I get it - genetics is cool, but America's healthcare system is a dumpster fire. You want to test your genes? Cool. Now pay $500 out of pocket while your insurance denies everything. Meanwhile, Big Pharma is laughing all the way to the bank. This isn't medicine - it's a subscription service for the rich. We need universal healthcare, not genetic VIP passes.
Jasmine Bryant
January 22, 2026 AT 00:07I work in a clinic and we started doing CYP2D6 testing for antidepressants last year. Honestly? Huge difference. One guy was on 100mg of sertraline for 8 months - no improvement, just dizziness. Turned out he was a poor metabolizer. Switched him to escitalopram, dose cut in half, and within 3 weeks he was hiking again. Not magic. Just science. But docs need training - most still think 'gene test = magic bullet'. It's not. It's a tool. Use it right.
Hilary Miller
January 23, 2026 AT 00:27My cousin in Nigeria got tested after her chemo almost killed her. Turns out she was DPYD-deficient. They adjusted her dose. She's alive today. This isn't a luxury. It's basic care.
Margaret Khaemba
January 24, 2026 AT 10:35So if I’m a rapid metabolizer of CYP2C19, does that mean I need more clopidogrel? Or just a different drug? I’m confused. I took Plavix for a stent and felt fine, but now I’m wondering if I got lucky. Also - can you get tested before you even get prescribed something? Like, as a preventive thing? I’d do it if it was $20.
Malik Ronquillo
January 25, 2026 AT 05:51My doctor said I'm a slow metabolizer for CYP2D6 and I should avoid codeine. So I switched to ibuprofen. Guess what? Still hurts. So now I just take two Advil and call it a day. Genetics is overrated. Just stop prescribing stupid drugs.