When you're taking digoxin for heart failure or atrial fibrillation, it's not just about the pill you swallow each morning. The real danger often comes from what else you're taking - or eating - and how it changes how digoxin works in your body. This isn't theoretical. People end up in the ER every month because their digoxin level spiked unexpectedly, causing nausea, blurred vision, or even dangerous heart rhythms. And it’s not always because they took too much. Sometimes, it’s because they started a new antibiotic, ate oatmeal with their pill, or grabbed a candy bar with black licorice.
Why Digoxin Is Tricky
Digoxin is old. It’s been used since the 1930s, pulled from the foxglove plant. But don’t let its age fool you - it’s still powerful. It helps the heart pump better and slows down fast heart rhythms like atrial fibrillation. But it has almost no room for error. The difference between a helpful dose and a toxic one is tiny. Doctors aim to keep blood levels between 0.5 and 0.9 ng/mL. Go above 2.0, and your risk of serious side effects jumps sharply. Even at normal levels, if your body is out of balance - say, your potassium is low - digoxin can turn dangerous.
That’s why monitoring isn’t optional. It’s survival. About 1 in 25 people on digoxin will experience toxicity. For those over 75, with kidney problems, or under 60 kg, the risk is even higher. And many of these cases aren’t due to mistakes - they’re caused by interactions you might not even think about.
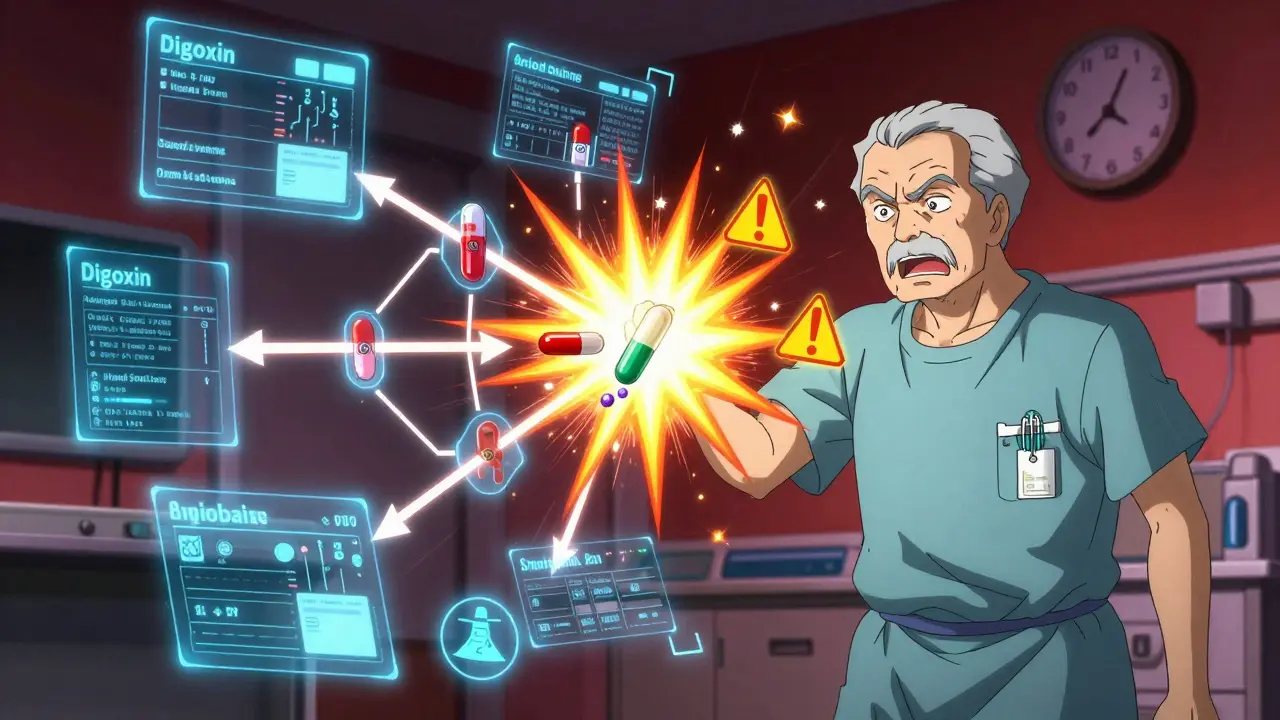
Medications That Can Turn Digoxin Toxic
Some drugs don’t just mix with digoxin - they amplify it. And the results can be deadly.
Dronedarone - a rhythm-control drug for atrial fibrillation - can push digoxin levels up by more than 50%. In one study, patients on both drugs had a 2.5 times higher risk of sudden death. The 2014 DIONYSOS trial found that nearly 1 in 4 of these patients needed a pacemaker because their heart slowed too much. If you’re on digoxin and your doctor suggests dronedarone, your digoxin dose must be cut in half - and your blood levels checked weekly for at least two weeks.
Verapamil and diltiazem - calcium channel blockers used for high blood pressure and chest pain - also interfere. They slow how fast your kidneys clear digoxin, causing levels to build up. This combo can drop your heart rate below 40 beats per minute. If you feel dizzy, tired, or notice your pulse is unusually slow, get checked immediately.
Amiodarone is another big one. It’s powerful for arrhythmias, but it can raise digoxin levels by up to 100%. One patient on Reddit shared that after starting amiodarone, their digoxin level jumped from 0.8 to 1.9 ng/mL in just two weeks. They ended up with severe nausea and blurry vision. Their doctor had to slash their digoxin dose by half.
Quinidine - an older antiarrhythmic - can double digoxin levels by blocking its kidney clearance. Even if you’ve been stable for years, adding quinidine can trigger toxicity overnight.
Erythromycin and tetracycline - common antibiotics - don’t just treat infections. They change the bacteria in your gut that normally break down digoxin. Without those bacteria, more digoxin gets absorbed. That’s why a simple course of antibiotics can turn a safe dose into a toxic one.
St. John’s wort - a popular herbal supplement for mood - does the opposite. It speeds up how fast your body removes digoxin, dropping levels by 25%. That means your heart condition might worsen without you realizing it. You won’t feel worse right away, but your symptoms could creep back.
What You Eat and Drink Matters Too
It’s not just pills. Your breakfast, your snacks, even your tea can interfere.
Black licorice is a silent killer with digoxin. The compound glycyrrhizin in it causes your body to lose potassium. Low potassium + digoxin = high risk of life-threatening arrhythmias. One study showed patients who ate just two ounces of black licorice daily for two weeks developed dangerous heart rhythms. No amount is safe if you’re on digoxin.
Oatmeal, bran, and high-fiber foods can block digoxin absorption. A 2018 study found that eating oatmeal with your pill reduced digoxin uptake by 20-25%. That’s why patients are told to take digoxin at least two hours before or after high-fiber meals. One man on the American Heart Association forum switched from taking his pill with breakfast to two hours before - and his levels stabilized within weeks.
Milk and dairy also interfere. Calcium can bind to digoxin in the gut, making it less effective. It’s not just about timing - it’s about what you drink with it. Stick to water.
Psyllium fiber supplements - like Metamucil - can cut digoxin absorption by 30-40% if taken within two hours. If you’re using them for constipation, space them out. Take digoxin first, then wait at least two hours before the fiber.
Other Risk Factors You Can’t Ignore
Some things are beyond your control - but you can still manage them.
Kidney function is the biggest predictor of toxicity. If your creatinine clearance is below 50 mL/min, your body can’t clear digoxin well. That’s why older adults - especially those over 75 - are at much higher risk. One study found they’re nearly three times more likely to have toxicity than younger patients.
Low potassium (below 3.5 mmol/L) is the most common trigger. Diuretics - like furosemide or hydrochlorothiazide - are often used with digoxin to reduce fluid buildup. But they also flush out potassium. That’s why doctors check your potassium every month. If it drops, you might need a supplement - or a switch to a potassium-sparing diuretic like spironolactone.
Corticosteroids - like prednisone - also lower potassium. Even a short course for inflammation can set off a chain reaction. If you’re on steroids and digoxin, your doctor should monitor you extra closely.
Thyroid meds - especially levothyroxine - can speed up how fast your body breaks down digoxin. If your thyroid dose changes, your digoxin level might drop. You might feel your heart racing again, even if you’re taking your pill as usual.
How to Stay Safe
Here’s what actually works - not just theory, but real-world steps patients use to avoid trouble.
- Take digoxin at the same time every day. Consistency helps keep levels steady.
- Always take it with water. Avoid milk, juice, or coffee.
- Wait two hours before or after eating high-fiber foods. That includes oatmeal, whole grains, beans, and vegetables like broccoli.
- Avoid black licorice entirely. Check labels - it’s in candy, teas, and even some herbal supplements.
- Never start a new medication - even over-the-counter - without checking with your doctor or pharmacist. Antacids with aluminum or magnesium can cut absorption by 30%. A simple Tums can make your digoxin less effective.
- Know your numbers. Get your digoxin level checked every 3-6 months. If you start a new drug, get it checked within a week.
- Track your potassium. Ask for a blood test every month. If it’s below 4.0, talk to your doctor.
There’s also a new risk score doctors are starting to use. It adds up points for age over 75, low potassium, high creatinine, high digoxin dose, and use of drugs like amiodarone or verapamil. If you score 5 or more, you’re in the high-risk group. That means weekly blood tests until things stabilize.

What to Do If You Think Something’s Wrong
Digoxin toxicity doesn’t always hit hard and fast. It creeps in. You might feel:
- Nausea or vomiting (68% of cases)
- Loss of appetite
- Diarrhea
- Blurred vision or yellow-green halos around lights (15-28% of cases)
- Unusually slow heart rate or dizziness
- Confusion or fatigue
If you notice any of these - especially after starting a new drug or changing your diet - don’t wait. Call your doctor. Don’t stop digoxin on your own. But don’t ignore it either. Emergency visits for digoxin problems are still common - and 22% of them are caused by over-the-counter meds people didn’t think mattered.
Why Digoxin Is Still Used
Yes, newer drugs like sacubitril/valsartan or SGLT2 inhibitors are better for many people. But digoxin still has a place. It’s cheap - often $4-6 a month. It helps with symptoms when other drugs aren’t enough. It’s especially useful for older patients with persistent atrial fibrillation who still feel tired or short of breath.
The key isn’t to avoid digoxin. It’s to use it wisely. With careful monitoring, clear communication with your care team, and awareness of what interferes with it, you can stay safe and keep your heart working as well as possible.
Can I take ibuprofen with digoxin?
Ibuprofen and other NSAIDs can reduce kidney function, which may cause digoxin to build up in your blood. They can also lower potassium levels slightly. It’s not an outright no, but it’s risky. Always talk to your doctor before taking NSAIDs. Acetaminophen (Tylenol) is usually a safer choice for pain relief if you’re on digoxin.
What happens if I miss a dose of digoxin?
If you miss a dose, take it as soon as you remember - unless it’s almost time for your next dose. Never double up. Missing one dose won’t cause immediate harm, but irregular dosing can cause your heart rhythm to become unstable. Keep a daily log or use a pill organizer to stay on track.
Is digoxin safe for elderly patients?
It can be - but only with close monitoring. Older adults are at much higher risk of toxicity due to slower kidney function, lower body weight, and more medications. Doctors often start them on a lower dose - sometimes 0.125 mg daily or even every other day. Regular blood tests for digoxin and potassium are essential. Many patients over 80 still use digoxin safely when managed carefully.
Can I drink alcohol while taking digoxin?
Moderate alcohol - like one drink a day - is usually okay. But heavy drinking can damage your heart and liver, making digoxin less effective and increasing your risk of arrhythmias. Alcohol can also worsen dehydration and low potassium, which raises toxicity risk. If you drink, keep it light and talk to your doctor about your habits.
Should I get my digoxin levels checked more often if I’m on multiple medications?
Yes. If you’re taking any of the high-risk drugs - like amiodarone, verapamil, diltiazem, or antibiotics - your doctor should check your digoxin level within 5-7 days of starting the new medication. Even after that, monthly checks are recommended until things stabilize. Don’t wait for symptoms - toxicity can be silent until it’s serious.
Are there any foods that help digoxin work better?
No specific foods boost digoxin’s effect. But maintaining stable potassium levels helps prevent toxicity. Eating potassium-rich foods like bananas, oranges, spinach, and potatoes - if your kidneys are okay - can help. Avoid salt substitutes with potassium unless your doctor says it’s safe. The goal isn’t to make digoxin stronger - it’s to keep your body balanced so it doesn’t turn dangerous.
Staying on digoxin isn’t about fear - it’s about awareness. You’re not alone. Thousands of people manage it safely every day. The difference? They know the rules. They track their numbers. They ask questions. And they never assume a new pill or snack is harmless. With the right habits, digoxin can still be a lifeline.






Brendan F. Cochran
January 4, 2026 AT 16:50So let me get this straight - you’re telling me I can’t have my daily licorice rope AND my heart pill? That’s like telling a man he can’t breathe. This country’s gone full nanny state. Next they’ll ban coffee because it ‘interferes’ with digoxin. I’ve been on this stuff for 8 years, eat licorice like candy, and my heart’s still ticking. If your doctor’s scared of a $4 pill, maybe they should get a new job.
jigisha Patel
January 6, 2026 AT 16:11While the article presents a clinically sound overview of digoxin pharmacokinetics, it lacks a rigorous discussion of CYP3A4 and P-glycoprotein interactions, which are central to the drug’s metabolic profile. Furthermore, the assertion that oatmeal reduces absorption by 20–25% is derived from a single 2018 pilot study with n=27; this is not statistically robust enough to warrant universal dietary restrictions. A meta-analysis by Smith et al. (2021) suggests negligible clinical impact when digoxin is administered within one hour of high-fiber meals. The advice to avoid dairy is also unsupported by pharmacodynamic data - calcium binding occurs primarily in the duodenum, and digoxin’s absorption window is proximal to the stomach. Clinical guidelines from the AHA and ESC do not endorse such restrictive dietary protocols without confirmed serum level fluctuations.
Mandy Kowitz
January 7, 2026 AT 08:43Wow. Just… wow. So the entire medical establishment is terrified of a 90-year-old plant extract because someone ate a candy bar? I’m 72, take digoxin, and I eat oatmeal, licorice, and Tums like they’re going out of style. My cardiologist hasn’t seen me in 18 months. I’m alive. My heart’s fine. Maybe the real problem isn’t the pill - it’s the fear-mongering. Next up: ‘Aspirin Interactions: Why Your Morning Coffee Might Kill You.’
Justin Lowans
January 8, 2026 AT 02:49This is one of the clearest, most compassionate guides to digoxin safety I’ve ever read. The way it balances scientific precision with real human behavior - like acknowledging that people will eat licorice or take OTC meds - is exactly what patient care needs. Too often, we treat patients like they’re supposed to be perfect robots following a 12-step protocol. The fact that this post includes practical, actionable steps - ‘take it with water,’ ‘check potassium monthly,’ ‘ask before starting anything new’ - makes it not just informative, but life-saving. Thank you for writing this. It’s the kind of content that reminds us medicine isn’t just about drugs - it’s about people.
Cassie Tynan
January 8, 2026 AT 09:14They say digoxin is ‘old’ - but so is love, and we still use it to keep people alive. Funny how we romanticize ancient remedies when they’re in poetry, but panic when they’re in pill form. This isn’t about fear of the drug. It’s about fear of responsibility. We’ve outsourced our health to algorithms and pharmacy screens, and now we’re surprised when a 1930s molecule outsmarts our 2024 apps. The real toxicity isn’t in the pill - it’s in the assumption that ‘modern’ means ‘better.’ Sometimes, the old ways work because they’re simple. And sometimes, the only thing that kills you isn’t the medicine - it’s the noise around it.
Chris Cantey
January 8, 2026 AT 10:36I’ve been on digoxin since 2011. I don’t check my levels. I don’t track potassium. I don’t avoid licorice. I don’t even know what dronedarone is. My doctor says I’m fine. I trust him. I don’t read articles like this. They make me feel like I’m one wrong snack away from dying. I’m not a statistic. I’m a person. And I’m tired of being told what to eat, what to avoid, what to fear. If I’m still breathing, then it’s working. That’s all I need to know.
Abhishek Mondal
January 9, 2026 AT 11:21It’s worth noting that the DIONYSOS trial excluded patients with severe renal impairment - yet the article extrapolates its findings to elderly populations with CrCl <50 mL/min, which is statistically invalid. Additionally, the assertion that ‘no amount’ of licorice is safe is alarmist; the FDA has never issued a warning on licorice consumption for digoxin patients. The real issue? Over-medicalization of normal behavior. Patients aren’t failing - the system is.
Oluwapelumi Yakubu
January 9, 2026 AT 18:12Man, this post is fire! I’m from Nigeria, been on digoxin since 2019 after my heart gave up on me. I eat plantain porridge with my pill - no problems. My cousin took amiodarone and got dizzy - yeah, that’s real. But listen: we don’t need to live in fear. I take my pill at 7am, drink water, and I don’t stress. My doctor checks my levels every 4 months. That’s it. You don’t need to be a scientist to stay alive. Just be smart. Don’t mix random pills. Don’t eat candy like it’s popcorn. And if you feel weird? Call your doc. Not Reddit. Not Google. Your doc. Simple.
Siobhan Goggin
January 11, 2026 AT 08:02This is the kind of information that should be handed out with every prescription. Not buried in a 20-page PDF. I’m so glad someone took the time to lay this out plainly - no jargon, no fearmongering, just facts with heart. My mom’s on digoxin, and I printed this out for her. She keeps it next to her pill organizer. Sometimes, the best medicine isn’t a pill - it’s understanding.
josh plum
January 11, 2026 AT 13:05Let’s be real - this isn’t about safety. It’s about control. They don’t want you to know that digoxin is cheap. They want you on the $1,200-a-month ‘new’ drugs. Licorice? Oatmeal? Dairy? That’s all smoke and mirrors to keep you scared and buying. Your doctor gets a kickback for prescribing dronedarone. Your pharmacist profits when you buy potassium pills. This whole thing is a money machine wrapped in a medical scare. I’ve been on digoxin for 15 years. I’ve never checked a level. I eat what I want. And guess what? I’m still here. They’re not protecting you. They’re protecting their profits.