Lactulose Dosing Calculator
This tool helps calculate the appropriate lactulose dose based on stool frequency and side effects as recommended by clinical guidelines.
Recommended Action
Please fill out the form to get dose recommendations.
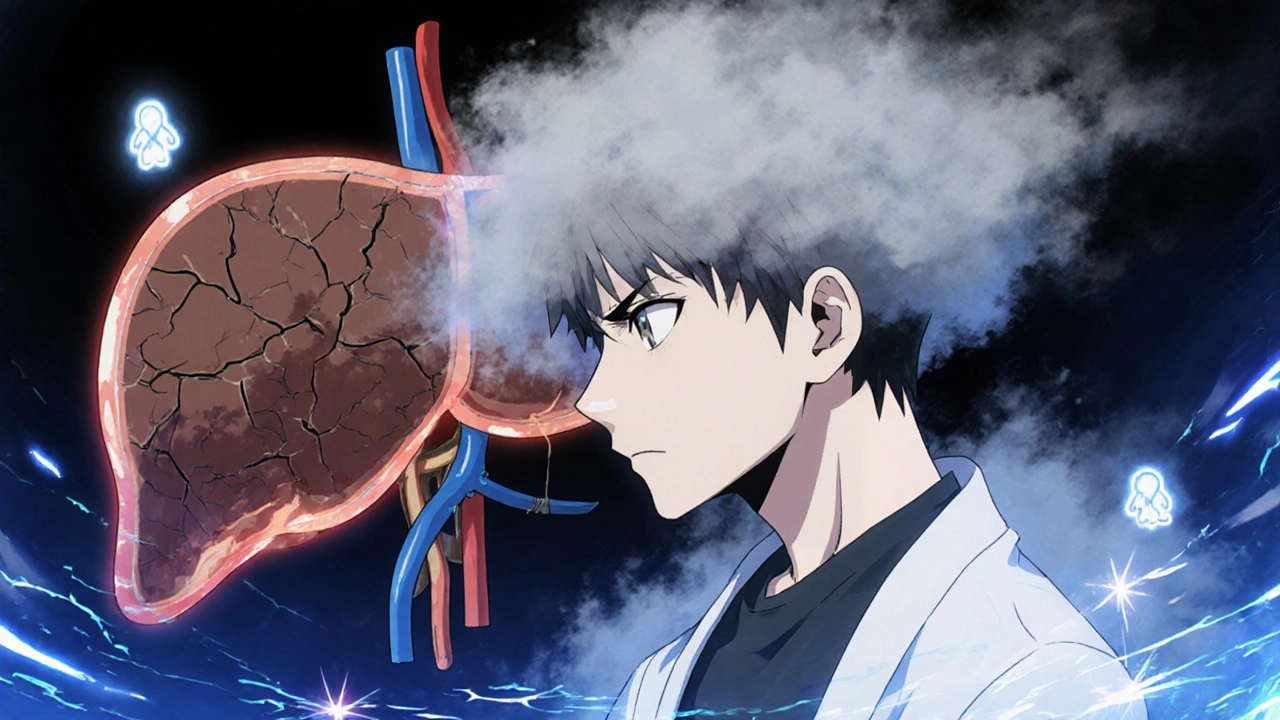
When the liver starts to fail, a confusing cloud of mental changes can appear overnight. This condition is called Hepatic Encephalopathy is a neuropsychiatric syndrome that arises when the liver can no longer detoxify harmful substances, especially ammonia. The most widely used remedy is Lactulose is a synthetic disaccharide that works inside the gut to trap ammonia and lower its blood level. In everyday language, lactulose turns a noisy, toxic gut into a quiet, safe one, letting the brain clear the fog. Below you’ll find a step‑by‑step guide to why lactulose matters, how to use it correctly, what to watch for, and when other drugs might be better.
What Exactly Is Hepatic Encephalopathy?
Hepatic Encephalopathy (HE) is not a single disease but a spectrum of brain dysfunction that follows chronic liver damage, most often cirrhosis. It can swing from subtle lapses in concentration (called minimal HE) to full‑blown coma. The root cause is the buildup of neurotoxins-chiefly ammonia-produced by gut bacteria and then dumped into the bloodstream because the damaged liver can’t convert them into urea.
Key clinical signs include:
- Confusion, forgetfulness, or trouble with simple tasks.
- Slurred speech (often described as “asterixis” or hand‑flapping).
- Sleep‑wake cycle reversal.
- Personality changes, irritability, or even hallucinations.
Doctors grade HE with the West Haven criteria, ranging from Grade 0 (no detectable changes) to Grade 4 (coma). The grading helps decide how aggressive the treatment should be.
Why Lactulose Is the First‑Line Choice
Lactulose has been the backbone of HE therapy for more than four decades. Its popularity isn’t just tradition-clinical trials repeatedly show it reduces hospital admissions and improves cognition. The drug works through three intertwined mechanisms:
- Acidification of the colon: Lactulose is metabolised by gut bacteria into lactic and acetic acids. The resulting lower pH converts free ammonia (NH₃) into ammonium (NH₄⁺), a charged molecule that cannot cross the gut wall easily.
- Prebiotic effect: The sugar feeds beneficial bacteria, shifting the microbial balance away from ammonia‑producing species such as Proteus and Enterobacter.
- Osmotic laxative action: By pulling water into the colon, lactulose speeds up bowel movements, hauling out trapped ammonia before it can be reabsorbed.
Because it tackles ammonia at its source, lactulose works even when other treatments (like antibiotics) fail.
Starting Lactulose: Dosage, Formulations, and Administration
Most patients begin with the liquid formulation (20 g per 100 ml). The goal is to produce 2-3 soft stools per day-enough to flush toxins without causing dehydration.
| Starting Dose | Adjustment Target | Maximum Recommended Dose |
|---|---|---|
| 15 ml (≈3 g) orally every 12 hours | 2-3 soft stools per day | 45 ml (≈9 g) three times daily |
| Increase by 5-10 ml every 1-2 days if stool frequency is low | Maintain soft, non‑watery stools | Do not exceed 60 ml per dose |
For patients who cannot swallow liquids, a powder that reconstitutes in water is available. Tablets exist in some markets, but they tend to be less well‑absorbed and may need higher doses.
Important administration tips:
- Take lactulose with food to lessen abdominal cramping.
- Measure doses with a calibrated syringe or cup-not a kitchen spoon.
- Check the label: some formulations contain sorbitol, which can worsen diarrhea in sensitive individuals.

Monitoring Effectiveness and Spotting Side Effects
Therapeutic success is judged by two practical markers:
- Clinical response: Improvement in mental status within 48-72 hours.
- Stool frequency: Consistent soft stools (2-4 per day) indicate adequate dosing.
If there’s no change after five days, consider the following:
- Non‑adherence or under‑dosing.
- Concurrent infection, gastrointestinal bleed, or electrolyte imbalance that can mask improvement.
- Need for adjunct therapy (rifaximin, probiotics, or zinc supplementation).
Common side effects are generally mild:
- Flatulence and bloating (often a sign of bacterial fermentation).
- Diarrhea if the dose is too high-watch for signs of dehydration (dry mouth, dizziness).
- Rarely, electrolyte disturbances (low potassium) in patients with chronic watery stools.
When severe diarrhea persists, reduce the dose by 5 ml and reassess after 24 hours.
How Lactulose Stacks Up Against Other HE Therapies
While lactulose remains first‑line, clinicians sometimes add or switch to other agents. Below is a quick comparison of the most common options.
| Feature | Lactulose | Rifaximin | Probiotic (e.g., VSL#3) |
|---|---|---|---|
| Mechanism | Acidifies colon, osmotic laxative | Gut‑specific antibiotic that reduces ammonia‑producing bacteria | Introduces beneficial microbes, modestly lowers ammonia |
| Cost (US, 2025) | ~$30/month (generic) | ~$300/month (brand) | ~$100/month (high‑potency blend) |
| Evidence level | Class I (randomized controlled trials) | Class I (large multicenter trials) | Class II (smaller trials, mixed results) |
| Typical side effects | Diarrhea, gas, cramps | nausea, mild abdominal pain | Bloating, rare infection in immunocompromised |
| Use case | All grades of HE, first‑line | Refractory HE or adjunct to lactulose | Adjunct, especially in patients intolerant to lactulose |
Guidelines from the American Association for the Study of Liver Diseases (AASLD, 2023) recommend lactulose plus rifaximin for patients who have had two or more HE-related hospitalisations in the past year. The combination cuts recurrence by roughly 45% compared with lactulose alone.
Practical Checklist for Patients and Caregivers
- Measure each dose accurately with a medical syringe.
- Aim for 2-3 soft stools daily; adjust dose if you’re constipated.
- Stay hydrated-drink at least 1.5 L of water per day unless your doctor says otherwise.
- Monitor mental status: note any confusion, sleep pattern changes, or asterixis.
- Report severe diarrhea, vomiting, or electrolyte issues to your clinician promptly.
- Keep a medication log to show adherence during follow‑up visits.

Frequently Asked Questions
Can lactulose be used in children with hepatic encephalopathy?
Yes. Pediatric dosing starts at 0.5 ml/kg every 12 hours and is titrated to stool frequency, just like in adults. Close monitoring is essential because children are more prone to dehydration.
Is it safe to combine lactulose with alcohol?
Alcohol worsens liver injury and can trigger HE episodes, so it should be avoided entirely while on lactulose. Even modest drinking can offset the drug’s benefits.
How long do I need to stay on lactulose?
Most patients remain on a maintenance dose for life, because cirrhosis is irreversible. If you achieve a stable stool pattern and no HE episodes for six months, your doctor may trial a dose reduction.
What should I do if I miss a dose?
Take the missed dose as soon as you remember, unless it’s almost time for the next scheduled dose. In that case, skip the missed one and resume the regular schedule-don’t double up.
Are there any foods I should avoid while taking lactulose?
High‑protein meals can increase ammonia production, so many clinicians suggest a moderate‑protein diet (0.8‑1.0 g/kg/day) rather than a very high‑protein regimen. Fiber‑rich foods help keep bowel movements regular.
When to Call Your Healthcare Provider
Even with the best regimen, HE can flare up suddenly. Contact your doctor or go to the emergency department if you notice any of the following:
- Rapid worsening of confusion or disorientation.
- New onset of asterixis or inability to hold a cup steady.
- Severe, watery diarrhea lasting more than 48 hours.
- Signs of dehydration: dry mouth, low urine output, dizziness.
- Yellowing of the skin that suddenly deepens (possible worsening liver failure).
Early intervention can prevent a trip to intensive care and may save lives.
Bottom Line
For anyone dealing with liver‑related brain fog, Lactulose remains the cheapest, most studied, and most effective first‑line therapy. Understanding how to dose it, watch for side effects, and combine it with other agents when needed turns a complex medical problem into a manageable daily routine.





hema khatri
October 23, 2025 AT 15:19Lactulose is the real superhero for liver patients!!! It traps ammonia in the gut, turns toxic clouds into clear skies, and keeps the brain fog at bay. You just need to keep the dosage steady, otherwise the benefits disappear, so measure it carefully!!
Jennell Vandermolen
October 24, 2025 AT 13:32Sticking to the recommended 2‑3 soft stools a day makes a huge difference; it shows the dose is right and the brain can recover. Remember to use a proper measuring syringe, not a kitchen spoon, to avoid under‑ or overdosing. Consistent monitoring helps you and your doctor catch any slip early.
Mike Peuerböck
October 25, 2025 AT 11:45Esteemed colleagues, the pharmacodynamic profile of lactulose warrants its primacy as first‑line therapy for hepatic encephalopathy; its triadic mechanism-colon acidification, prebiotic modulation, and osmotic laxation-synergistically attenuates systemic ammonia concentrations. Empirical evidence amassed over four decades substantiates its efficacy in reducing hospital readmissions and enhancing neurocognitive outcomes. Accordingly, adherence to titrated dosing regimens is indispensable for therapeutic success.
Simon Waters
October 26, 2025 AT 08:59Some people think the push for lactulose is just big pharma trying to sell more sugar‑based drugs, but the science is clear that it works by lowering ammonia. Still, it's worth staying aware of who profits.
Kajal Gupta
October 27, 2025 AT 07:12Honestly, lactulose can feel like a weird syrup, but once you get the hang of the dose, it’s like giving your gut a gentle clean‑up crew. Keep an eye on the stool count; two to three soft poops a day means you’re on the right track, and the mental fog will start lifting.
Zachary Blackwell
October 28, 2025 AT 05:25It is evident that the medical establishment subtly downplays alternative modalities while glorifying lactulose as the sole savior, despite emerging data on microbiome‑targeted therapies that could eclipse its modest efficacy. The subtle bias in guidelines should prompt us to scrutinize the underlying interests.
prithi mallick
October 29, 2025 AT 03:39When we ponder the liver’s role as a filter, we see lactulose as a humble bridge between gut and mind, reminding us that balance is a delicate artt. Stay gentle with your dosing, and let the body’s wisdom guide the healing journey.
Michaela Dixon
October 30, 2025 AT 01:52Lactulose remains the cornerstone of hepatic encephalopathy management, and its prolonged use has been validated across numerous clinical trials. The mechanism hinges on acidifying the colon, which converts free ammonia into the non‑absorbable ammonium ion. By feeding beneficial bacterial populations, it also shifts the microbiome away from ammonia‑producing species. Its osmotic effect ensures rapid transit, flushing trapped toxins before they can re‑enter circulation. Patients who achieve the target of two to three soft stools per day often notice an early improvement in clarity within 48 hours. Consistent dosing is essential; both under‑dosing and excessive dosing can compromise effectiveness. Measuring with a calibrated syringe eliminates the variability that spoons introduce. Hydration plays a complementary role, as adequate fluid intake supports laxative action while preventing dehydration. Side effects such as bloating, gas, or mild diarrhea are usually dose‑related and resolve with modest adjustments. If diarrhea becomes severe, a reduction of 5 ml typically restores balance without losing therapeutic benefit. Monitoring mental status alongside stool frequency provides a practical bedside assessment of response. In refractory cases, adjunctive agents like rifaximin may be added, but lactulose alone suffices for many. Cost considerations favor lactulose, especially in resource‑limited settings, where generic formulations are affordable. Education of caregivers about measuring and adherence dramatically reduces readmission rates. Ultimately, the simplicity of lactulose, combined with its multifaceted action, makes it a uniquely effective tool in the battle against liver‑related brain fog.
James Gray
October 31, 2025 AT 00:05Keep it steady and the fog will lift fast.
Scott Ring
October 31, 2025 AT 22:19From my experience, mixing a little fruit juice with lactulose makes it easier to swallow and doesn’t affect its action, so give it a try if the taste bothers you.
Shubhi Sahni
November 1, 2025 AT 20:32Remember-measure every dose precisely!!! Keep hydrated, drink plenty of water!!! Watch for signs of dehydration, such as dry mouth or dizziness!!! Stay on top of your stool schedule, and you’ll keep the brain clear!!!