When your lungs start to feel heavy, your chest tightens, and breathing becomes a chore, it’s not just a bad cold. It could be pneumonia - and not all types are the same. Knowing whether it’s bacterial, viral, or fungal isn’t just academic; it determines whether you get antibiotics, antivirals, or something completely different. Misdiagnose it, and you risk worsening your condition or fueling antibiotic resistance. The CDC reports that nearly 30% of outpatient antibiotic prescriptions for respiratory infections are unnecessary - often because pneumonia types aren’t properly identified.
Bacterial Pneumonia: The Sudden Onset
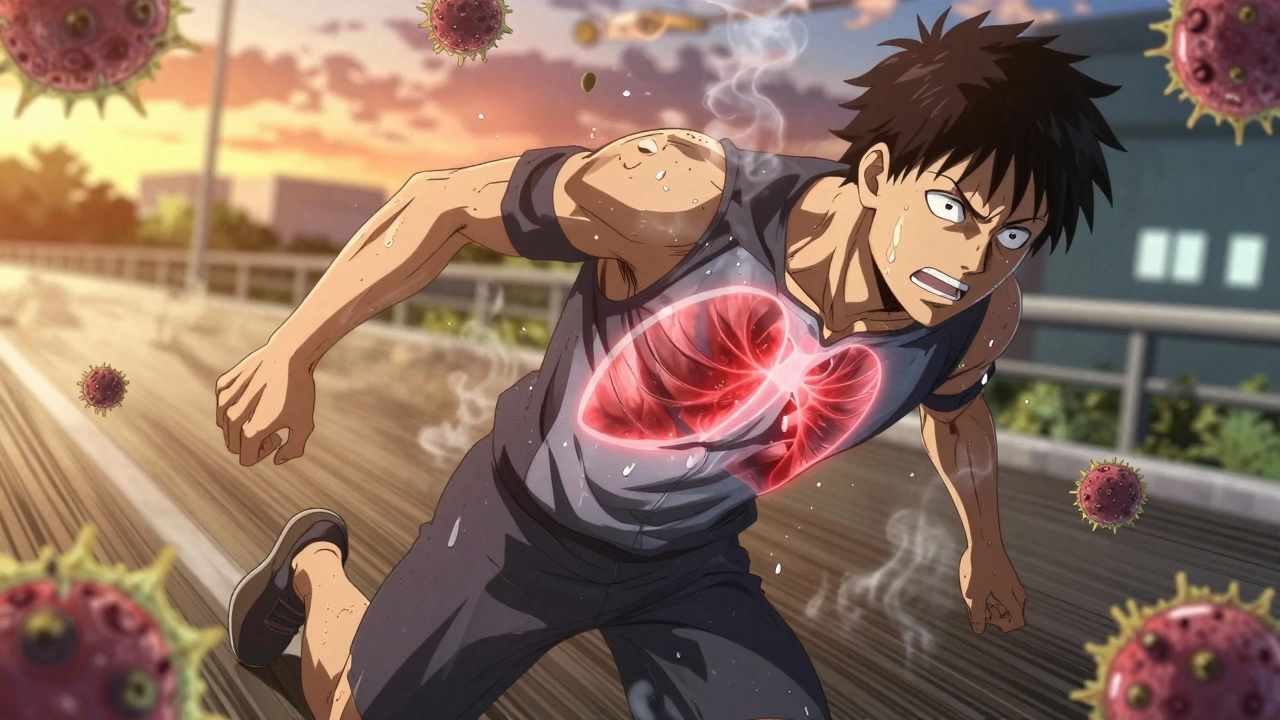
Bacterial pneumonia hits fast. One day you might feel fine; the next, you’re running a high fever - 102°F to 105°F - with chills, rapid breathing, and a cough that brings up thick, yellow, green, or even bloody mucus. Chest pain is sharp and gets worse when you cough or take a deep breath. Your lips or fingernails might turn blue because your body isn’t getting enough oxygen. The most common culprit? Streptococcus pneumoniae. It’s responsible for over half of all community-acquired bacterial pneumonia cases. Other bacteria like Haemophilus influenzae, Staphylococcus aureus, and Mycoplasma pneumoniae (which causes milder "walking pneumonia") also show up often. Legionella pneumophila, the germ behind Legionnaires’ disease, is rarer but more dangerous. On a chest X-ray, bacterial pneumonia usually shows up as one solid white patch - called lobar consolidation - in one part of the lung. That’s because the infection fills the air sacs with fluid and immune cells, clumping them together. Doctors can often tell it’s bacterial just by how quickly symptoms escalate and what the scan looks like. Treatment? Antibiotics. Penicillin, macrolides like azithromycin, or fluoroquinolones like levofloxacin are common choices. But timing matters. The sooner you start the right antibiotic, the better your chances. Delayed treatment increases the risk of complications like lung abscesses or sepsis.Viral Pneumonia: The Slow Burn
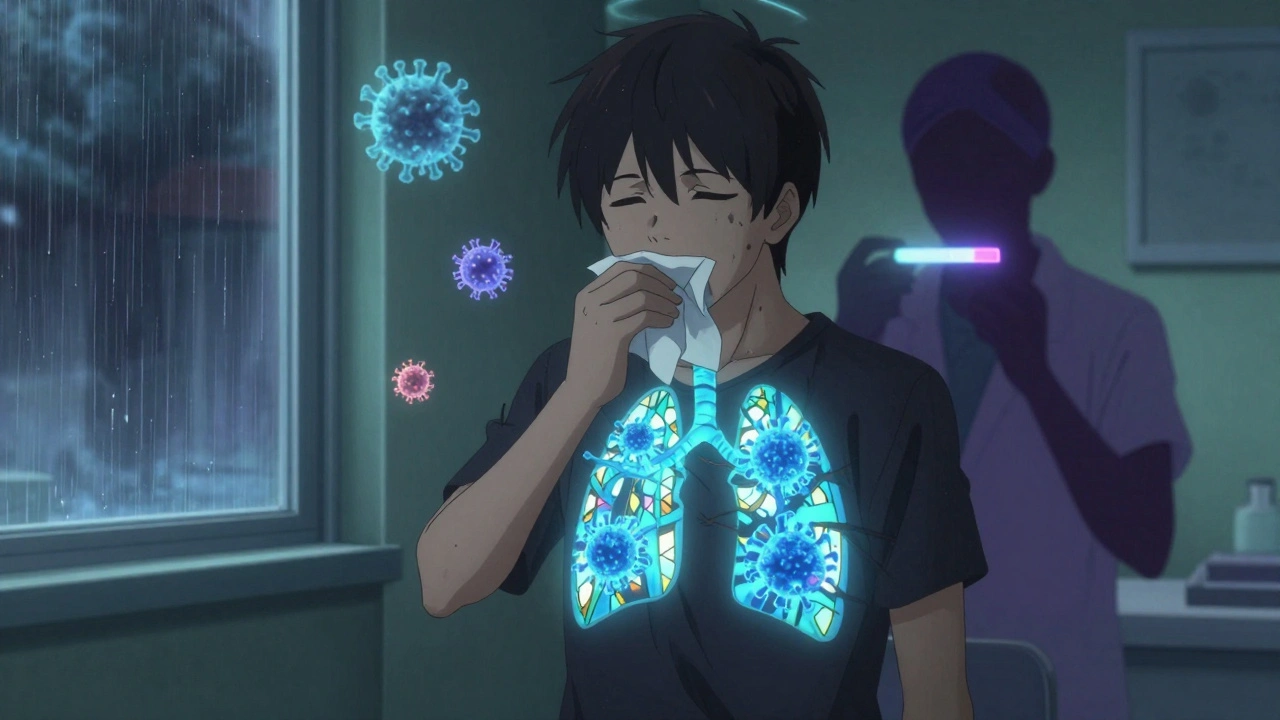
Viral pneumonia doesn’t come out of nowhere. It creeps in. You start with a runny nose, sore throat, maybe a low-grade fever - the kind you’d write off as a cold. Then, after three to five days, things shift. Your cough gets worse. You feel exhausted. Your muscles ache. You might have a headache. Fever stays mild, usually between 100°F and 102°F. This type is often caused by influenza A and B, RSV (respiratory syncytial virus), rhinovirus, or SARS-CoV-2 (the virus behind COVID-19). In fact, during flu season, up to 30% of pneumonia cases are viral. RSV is especially common in young children and older adults. Unlike bacterial pneumonia, viral pneumonia doesn’t show up as one solid white patch on an X-ray. Instead, you’ll see a hazy, scattered pattern across both lungs - called interstitial infiltrates. That’s because the virus attacks the walls of the air sacs and tiny airways, causing inflammation and swelling throughout the lung tissue. Antibiotics won’t help here. They do nothing to viruses. Instead, treatment focuses on rest, fluids, fever reducers, and oxygen support if needed. For flu, antivirals like oseltamivir (Tamiflu) can help if taken within 48 hours of symptoms starting. For severe COVID-19 pneumonia, remdesivir may be used in hospitals. Here’s the big risk: viral pneumonia can open the door to a second infection. About 25-30% of people with severe flu or COVID-19 pneumonia develop a secondary bacterial infection - usually from Streptococcus pneumoniae or Staphylococcus aureus. That’s why doctors watch closely for worsening symptoms after the first few days.Fungal Pneumonia: The Hidden Threat
Fungal pneumonia is rare in healthy people. But if your immune system is weakened - whether from HIV, chemotherapy, organ transplants, or long-term steroid use - you’re at risk. It’s not something you catch from a sneeze. You breathe it in from the environment. In the U.S., three fungi cause most cases:- Coccidioides - found in dry soil in the Southwest (Arizona, California). Causes Valley fever. About 20,000 cases a year.
- Histoplasma capsulatum - lives in bird and bat droppings. Common in the Ohio and Mississippi River valleys. Around 65% of people in these areas have been exposed.
- Blastomyces dermatitidis - grows in moist soil near rivers and lakes. Causes blastomycosis. About 1-2 cases per 100,000 people annually.
How Doctors Tell Them Apart
Distinguishing between these types isn’t guesswork anymore. Here’s what doctors use:| Feature | Bacterial | Viral | Fungal |
|---|---|---|---|
| Onset | Sudden (hours to 1 day) | Gradual (3-5 days) | Gradual (days to weeks) |
| Fever | High (102-105°F) | Mild to moderate (100-102°F) | Moderate to high |
| Cough | Productive, colored sputum | Dry, worsening over time | Dry or phlegmy |
| Chest X-ray | Lobar consolidation (one area) | Bilateral interstitial infiltrates | Nodules, patchy infiltrates |
| Common Pathogens | Streptococcus pneumoniae, Haemophilus | Influenza, RSV, SARS-CoV-2 | Coccidioides, Histoplasma, Blastomyces |
| Treatment | Antibiotics | Supportive care, antivirals if early | Antifungals |
Lab tests help too. Blood cultures, sputum tests, and rapid antigen tests can point to bacteria. PCR panels now detect over 20 viruses and fungi from a single nasal swab - with 95% accuracy. That’s a game-changer. No more guessing.
Prevention: What Actually Works
You can’t avoid every germ, but you can reduce your risk:- Pneumococcal vaccines - Prevnar 20 (approved in 2021) protects against 20 strains of Streptococcus pneumoniae. It’s recommended for all kids under 2, adults 65+, and people with chronic conditions. Studies show it cuts pneumonia risk by 60-70% in children and 80% in adults.
- Flu shot - Reduces pneumonia risk by 40-60% during flu season. Even if you get the flu, it’s less likely to turn into pneumonia.
- COVID-19 vaccines - Reduce pneumonia risk by up to 90% in the first few months after vaccination.
- For fungal pneumonia - Avoid disturbing soil in endemic areas. Wear a mask when gardening, cleaning chicken coops, or working in caves. If you’re immunocompromised, talk to your doctor about preventive antifungals in high-risk zones.
Yet, vaccination rates are still too low. Only 68% of adults over 65 have had the pneumococcal shot. That means over 1 in 3 older adults are unprotected. For flu shots, the rate is better - around 55% - but still far from where it should be.

Why Getting It Right Matters
Pneumonia kills about 50,000 people in the U.S. every year. Bacterial pneumonia has a 5-7% death rate in hospitalized patients. Viral pneumonia kills 3-5%, but spikes to 9% in elderly flu patients. Fungal pneumonia? It’s deadlier - 10-15% mortality in people with weak immune systems. The real cost isn’t just lives lost. It’s money wasted. Every time someone gets antibiotics for a viral infection, we push bacteria toward resistance. The CDC says 30% of outpatient antibiotics are unnecessary. That’s 25 million prescriptions a year that don’t help - and might hurt. New tools are coming. Researchers are testing blood biomarkers that can tell bacterial from viral infections within hours - not days. If successful, this could cut inappropriate antibiotic use by 40%.When to See a Doctor
Don’t wait if you have:- Fever above 102°F that doesn’t break
- Coughing up blood or thick, colored mucus
- Difficulty breathing or rapid, shallow breaths
- Chest pain that worsens with breathing
- Lips or nails turning blue
- Confusion or dizziness (especially in older adults)
These aren’t signs to tough out. They’re red flags. Early diagnosis saves lives.
Can you have pneumonia without a fever?
Yes, especially in older adults, young children, or people with weakened immune systems. In these groups, pneumonia might only show up as confusion, fatigue, or a drop in appetite. A fever isn’t always present, so don’t rely on it alone to rule out infection.
Is viral pneumonia contagious?
Yes. Viral pneumonia spreads the same way as the virus that caused it - through coughs, sneezes, or touching contaminated surfaces. Influenza and COVID-19 are highly contagious. That’s why wearing a mask, washing hands, and staying home when sick helps prevent spread.
Can fungal pneumonia be caught from another person?
No. Fungal pneumonia isn’t contagious. You get it by inhaling spores from the environment - soil, bird droppings, or dust. You can’t catch it from someone else, even if they’re sick with it.
How long does it take to recover from pneumonia?
Recovery varies. Bacterial pneumonia often improves in 1-2 weeks with antibiotics, but fatigue can last weeks longer. Viral pneumonia may take 2-4 weeks to fully clear. Fungal pneumonia can require months of treatment, especially in immunocompromised people. Rest and hydration are key no matter the type.
Do I need a chest X-ray to diagnose pneumonia?
Not always, but it’s often needed. Doctors may diagnose based on symptoms and listening to your lungs. But if you’re severely ill, older, or not improving, a chest X-ray confirms pneumonia and helps determine the type. It also rules out other issues like a collapsed lung or tumor.
If you’ve had pneumonia before, you’re not immune. Repeat infections are common, especially if you smoke, have COPD, or are over 65. Stay up to date on vaccines, avoid smoking, and don’t ignore lingering symptoms. Your lungs are worth protecting.





Debbie Naquin
December 1, 2025 AT 20:14Pathogen-specific immune modulation is non-trivial in pneumonia etiology. The interstitial infiltrate pattern in viral cases reflects alveolar wall inflammation rather than alveolar exudate. This has direct therapeutic implications-antibiotics lack mechanism of action against viral cytopathology.
Moreover, the immunocompromised host fails to mount neutrophilic response, rendering classical radiographic markers unreliable. Fungal spore inhalation triggers granulomatous pathways-distinct from pyogenic consolidation. We need biomarkers beyond CRP and procalcitonin.
Margaret Stearns
December 2, 2025 AT 08:09thanks for this. i had pneumonia last year and no one told me fungal was even a thing. i live in ohio and used to clean out bird feeders. now i wear a mask. small change, big difference.
Erin Nemo
December 2, 2025 AT 18:19my grandpa got it without a fever and just kept saying he was tired. we thought he was just old. turns out it was bacterial. this post saved my aunt’s life-she went to the doc right away after reading this.
Rachel Stanton
December 4, 2025 AT 02:34Great breakdown. One thing to emphasize: even in healthy adults, viral pneumonia can lead to secondary bacterial infection. That’s why monitoring symptoms beyond day 5 is critical.
Also, for anyone in the Midwest or Southwest-don’t ignore a dry cough after digging in soil or visiting caves. Histoplasmosis and coccidioidomycosis are silent killers. Get tested if it lingers.
amit kuamr
December 5, 2025 AT 01:26in india we see mostly bacterial and viral pneumonia. fungal is rare unless patient is diabetic or on steroids. but doctors still give antibiotics first. no xray no test. just guess. this is why resistance is so bad here.
need better access to rapid pcr. not just in us.
Kelly Essenpreis
December 5, 2025 AT 14:20so you're telling me i should get a vaccine for something i might breathe in from dirt
next you'll say i need a shot for gravity
this is why america is broke. we vaccinate against nature now
James Allen
December 7, 2025 AT 07:26oh wow. so now we’re supposed to be scared of dirt and birds and soil
what’s next? a vaccine for oxygen? because breathing is clearly the real enemy here
and don’t get me started on how they’re pushing these shots like they’re candy at a parade. i’m not falling for it.
my grandpa lived to 92 and never got one of these fancy shots. he just breathed. and he won.
Amber-Lynn Quinata
December 8, 2025 AT 13:57omg i just realized i never got the pneumococcal shot 😭 i’m 58 and work in a garden center 🌿 so i’m basically a walking fungal spore magnet 🤢
going to book my appointment right now. thank you for the wake up call 🙏❤️
Scotia Corley
December 10, 2025 AT 03:40While the article presents a clinically sound overview, it omits a critical consideration: the socioeconomic disparity in diagnostic access. In rural and underinsured populations, chest X-rays and PCR panels remain inaccessible. The recommendation for biomarker-driven diagnosis is aspirational, not practical, for the majority of patients globally. Antibiotic overuse persists not due to ignorance, but due to systemic failure. Policy intervention, not patient education alone, will reduce unnecessary prescriptions. Until then, the burden falls disproportionately on those least equipped to navigate complex diagnostic pathways.