Probiotic Calculator for Antibiotic Therapy
Calculate Your Probiotic Strategy
Recommended Probiotic Strategy
When you’re on antibiotics, you know the deal: the infection starts to clear up, but then your stomach turns against you. Diarrhea, bloating, cramps - it’s like your gut is staging a protest. And it’s not just bad luck. Antibiotics don’t just kill the bad bacteria; they wipe out the good ones too. That’s where probiotics come in. But are they really helpful? And if so, how do you use them without making things worse?
Why Antibiotics Mess With Your Gut
Your gut is home to over 100 trillion bacteria. These microbes don’t just sit around - they help digest food, train your immune system, and even make vitamins. When you take antibiotics, especially broad-spectrum ones like amoxicillin or ciprofloxacin, they don’t distinguish between good and bad bugs. They hit everything. That’s why up to 30% of people on antibiotics end up with diarrhea. In hospitals, the risk jumps even higher. About 5 to 35% of patients develop Clostridioides difficile (C. diff) infections, a serious form of antibiotic-associated diarrhea that can lead to hospitalization or even death.How Probiotics Help - And What the Science Says
Probiotics are live bacteria or yeasts that can help restore balance in your gut. The most studied strains for antibiotic use are Lactobacillus rhamnosus GG, Saccharomyces boulardii, and certain Bifidobacterium species. These aren’t magic pills, but they’ve been shown to make a real difference. A major Cochrane review from 2020 looked at 2,454 people across 13 studies. Those who took probiotics while on antibiotics had just a 3.1% chance of developing C. diff diarrhea - compared to 11.6% in those who didn’t. That’s more than a 70% drop in risk. For general antibiotic-associated diarrhea, the benefit was still strong: probiotics cut the risk by about half in high-risk groups. Saccharomyces boulardii, a yeast probiotic, stands out. One 2018 meta-analysis found it reduced antibiotic diarrhea risk by 50%. L. rhamnosus GG, found in products like Culturelle, showed similar results. But not all probiotics work the same. Some multi-strain blends showed little to no benefit. The key isn’t just taking a probiotic - it’s taking the right one.Which Strains Actually Work?
Not all probiotics are created equal. Here’s what the evidence supports for antibiotic use:- Saccharomyces boulardii - Yeast-based, survives antibiotics, reduces diarrhea risk by up to 50%
- Lactobacillus rhamnosus GG - Well-studied, effective for both prevention and reducing duration of diarrhea
- Bifidobacterium lactis - Often paired with Lactobacillus in multi-strain formulas
- Lactobacillus acidophilus - Common in yogurt, but less effective alone than GG
When and How to Take Them
Timing matters. Antibiotics can kill probiotics if they’re taken at the same time. Most experts recommend spacing them out by 2 to 3 hours. Take your antibiotic, then wait a few hours before the probiotic. That gives the antibiotic time to do its job without wiping out the helpful bugs. Dose-wise, aim for 5 to 10 billion CFUs per day. Some products go higher - up to 50 billion - but there’s no proof more is better. Stick to the range that’s been studied. Take them daily during your antibiotic course and for at least 1 to 2 weeks after you finish. That gives your gut time to rebuild. Some probiotics work better on an empty stomach (like acid-resistant strains), others with food. Check the label. If it doesn’t say, take them with a light meal - it’s usually safe and helps reduce initial bloating.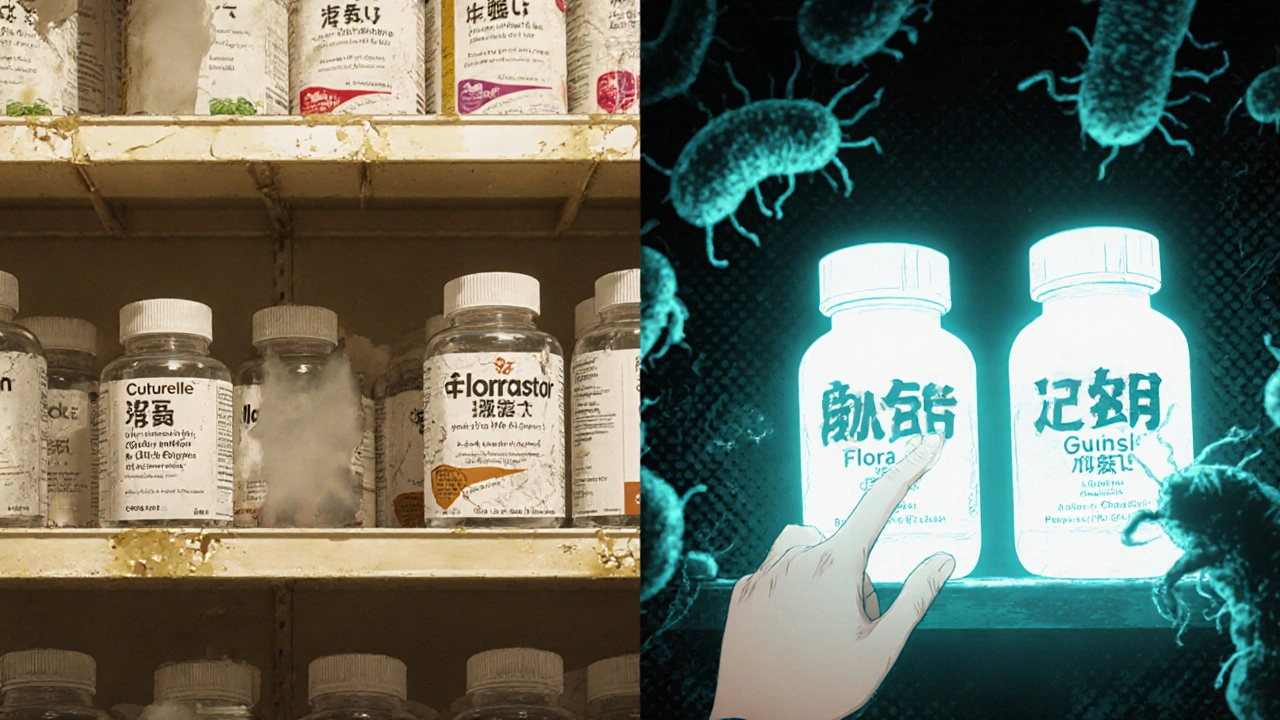
What About Side Effects?
Most people tolerate probiotics fine. But when you first start, you might feel bloated, gassy, or even a little constipated. That’s usually temporary - it’s your gut adjusting. If symptoms last more than a few days or get worse, stop and talk to your doctor. There’s a catch: probiotics aren’t risk-free. In rare cases, they’ve caused infections in people with weakened immune systems. There are documented cases of Lactobacillus and Saccharomyces entering the bloodstream, leading to sepsis or endocarditis. These are extremely rare in healthy people, but if you’ve had recent surgery, are on chemotherapy, have HIV, or use a central line, you should avoid probiotics unless your doctor says it’s safe.What’s on the Shelf - And What You Should Avoid
In the U.S., probiotics are sold as dietary supplements, not medicines. That means the FDA doesn’t test them for safety or effectiveness before they hit store shelves. A 2022 ConsumerLab test found 30% of probiotic products didn’t contain the number of live organisms listed on the label. Another 15% had extra bacteria not listed at all - some even contained harmful contaminants. Popular brands like Culturelle (L. rhamnosus GG) and Florastor (S. boulardii) are among the most trusted, with thousands of positive reviews. Amazon ratings for Culturelle sit at 4.2 out of 5 stars from over 12,500 reviews, with users frequently saying they “avoided diarrhea” while on antibiotics. But don’t trust marketing. Look for:- Specific strain names (e.g., L. rhamnosus GG, not just “Lactobacillus”)
- CFU count (5-10 billion is ideal)
- Expiration date (live cultures die over time)
- Reputable manufacturer (no vague claims like “supports immunity”)
Real People, Real Results
On Reddit, users in r/Probiotics share their experiences daily. One person on amoxicillin for a sinus infection took Culturelle twice daily, 3 hours after each dose. They had zero diarrhea. Another, on doxycycline for acne, tried a generic brand and got worse bloating. Switched to Florastor - symptoms disappeared. But not everyone wins. About 15% of negative Amazon reviews say “no effect.” Another 10% say symptoms got worse - often people with IBS or sensitive guts. Probiotics aren’t a cure-all. They work best for people who are otherwise healthy and taking antibiotics for a short time.
What Doctors Really Think
There’s disagreement. Harvard Health says probiotics “may help reduce common side effects.” The Cleveland Clinic says they’re “likely helpful” but warns about initial bloating. Meanwhile, Henry Ford Health System cautions that “evidence is slim” and advises talking to your doctor - especially if you’re immunocompromised. The International Scientific Association for Probiotics and Prebiotics (ISAPP) says probiotics may even improve antibiotic effectiveness by keeping the gut environment balanced. But they also stress: “Different strains do different things.” There’s no one-size-fits-all.The Bigger Picture
The global probiotic market is worth over $68 billion. In the U.S., nearly 4 million adults use probiotics specifically to manage antibiotic side effects. But without strict regulation, quality is hit or miss. The FDA released draft guidance in 2023 to improve oversight, but full rules won’t be in place until at least 2026. And here’s a twist: some studies suggest certain probiotics might actually delay gut microbiome recovery after antibiotics. One 2021 Nature study found that people who took probiotics took longer to return to their original bacterial balance than those who didn’t. That doesn’t mean avoid them - it means be smart. Use them to prevent diarrhea, not as a blanket fix for everything.Final Advice
If you’re on antibiotics and worried about your gut:- Choose a probiotic with a proven strain: L. rhamnosus GG or S. boulardii
- Take 5-10 billion CFUs daily
- Space it 2-3 hours after your antibiotic
- Keep taking it for 1-2 weeks after finishing your course
- Stop if you’re immunocompromised, critically ill, or have a central line - talk to your doctor first
- Don’t rely on yogurt alone - it doesn’t have enough live cultures or the right strains
Can I get enough probiotics from yogurt instead of supplements?
Most yogurt doesn’t contain enough live cultures or the right strains to help with antibiotic side effects. Even “live and active culture” yogurt typically has far fewer than 1 billion CFUs per serving, and the strains aren’t always proven for this use. Supplements are more reliable because they’re designed to deliver specific, tested strains in effective doses.
Do probiotics interfere with antibiotics?
They can - if you take them at the same time. Antibiotics kill bacteria, including the good ones in probiotics. Spacing them 2 to 3 hours apart prevents this. Some strains, like Saccharomyces boulardii, are yeasts and aren’t affected by antibiotics, so timing is less critical for those. But for bacterial probiotics, separation is key.
How long should I take probiotics after antibiotics?
Continue for at least 1 to 2 weeks after finishing your antibiotic course. Your gut microbiome doesn’t bounce back overnight. Studies show that taking probiotics beyond the antibiotic period helps stabilize the gut environment and reduces the chance of late-onset diarrhea or lingering bloating.
Are there any probiotics I should avoid?
Avoid probiotics if you’re immunocompromised, have a central IV line, recently had surgery, or are critically ill. Also avoid products without clear strain names, low CFU counts, or unknown manufacturers. Some cheap supplements contain unlisted or harmful microbes. Stick to well-researched brands with transparent labeling.
Can probiotics cause antibiotic resistance?
There’s no strong evidence that probiotics cause antibiotic resistance in humans. However, some lab studies show probiotic bacteria can transfer genes to other microbes - including harmful ones - under certain conditions. This is still being studied, but for healthy people taking probiotics as directed, the risk is considered extremely low.
What if I forget to take my probiotic at the right time?
If you take your probiotic right after your antibiotic, don’t panic. One missed window won’t ruin the benefit. Just take it as soon as you remember, and get back on schedule. Consistency matters more than perfection. Aim to space them out most days, but don’t stress over occasional overlap.






Johannah Lavin
November 19, 2025 AT 18:25OMG YES 🙌 I was on amoxicillin last month and thought I was gonna die from the cramps... took Culturelle like 3 hours after each dose and boom - zero drama. My gut thanked me. 🍃💖
Matthew Karrs
November 20, 2025 AT 09:12Probiotics? More like placebo pills sold by Big Yogurt. The FDA doesn’t regulate them, and 30% of products don’t even have what’s on the label. You’re just feeding bacteria that might turn on you later. Wake up.
Matthew Peters
November 20, 2025 AT 15:56I tried S. boulardii during my doxycycline round - worked like a charm. No diarrhea, just mild bloating for a day. But then I read that Nature study saying probiotics might slow microbiome recovery... now I’m confused. Do we really know what we’re doing?
Liam Strachan
November 20, 2025 AT 22:46Interesting read - thanks for laying it out so clearly. I’ve always just taken yogurt with my antibiotics, never thought about strain specificity. Guess I’ve been lucky. Might try Florastor next time. 😊
Gerald Cheruiyot
November 21, 2025 AT 15:38Science says one thing but biology says another. We treat the gut like a machine you can fix with a part. But it’s a living ecosystem. Maybe the real fix isn’t adding bugs but removing stress, sugar, and fear. Probiotics help? Maybe. But they’re not the answer - just a bandage.
Michael Fessler
November 21, 2025 AT 19:16Important note: CFU counts are meaningless without strain-level specificity. L. rhamnosus GG has documented translocation resistance and mucosal adherence - that’s why it works. Generic blends? Just sugar-coated filler. Also, avoid enteric-coated capsules unless you’re on PPIs - they’re overkill.
daniel lopez
November 23, 2025 AT 14:29They’re hiding the truth. Probiotics are a scam pushed by Big Pharma to keep you buying pills while they profit from your C. diff cases. They don’t want you to know that fasting and bone broth heal your gut better. Watch the documentary ‘Gut Betrayal’ - it’s all there.
Nosipho Mbambo
November 23, 2025 AT 19:33I tried this. I really did. Took the probiotic. Spaced it out. Followed all the rules. Still got diarrhea. So much for science. And now I’m out $25 and still on the toilet. Why do people even believe this?!
Katie Magnus
November 24, 2025 AT 22:00Probiotics? Please. That’s like putting a Band-Aid on a broken leg. Everyone’s obsessed with ‘gut health’ like it’s a TikTok trend. You don’t need supplements. Just eat real food. And stop buying into wellness marketing. It’s all nonsense.
King Over
November 26, 2025 AT 13:36Florastor saved me during my clindamycin round. Took it after meals. No issues. No drama. Just quiet gut. I don’t care what the studies say. My body knew what to do.
Ravi boy
November 26, 2025 AT 13:54bro i took a random indian brand probiotic with amoxi and it worked better than culturelle honestly. no idea why but my belly stopped crying. maybe the strains are same just cheaper? idk man
Ravinder Singh
November 27, 2025 AT 18:27For anyone reading this - don’t panic if you miss the 2-3 hour window. Your gut isn’t a Swiss watch. I’ve taken mine 30 mins after antibiotics and still avoided diarrhea. Consistency > perfection. And if you’re healthy? You’re probably fine. The real enemy is sugar, stress, and sleep deprivation - not missing a dose.