Most people don’t realize how quietly type 2 diabetes creeps in. You might feel tired more often. Thirstier than usual. Maybe you’re peeing more at night. But you blame it on stress, aging, or drinking too much coffee. By the time you notice the numbness in your feet or a wound that won’t heal, the disease has been working under the surface for years. Type 2 diabetes isn’t just about sugar-it’s a systemic breakdown in how your body uses energy, and it’s far more common than most think.
What’s Actually Happening in Your Body?
Type 2 diabetes isn’t caused by eating too much sugar. It’s caused by your body’s cells becoming resistant to insulin-the hormone that tells your muscles and fat to soak up glucose from your blood. At first, your pancreas works overtime, pumping out extra insulin to compensate. But over time, the beta cells that make insulin get worn out. By the time you’re diagnosed, you’ve already lost about half of your insulin-making capacity-and it keeps declining at 4-5% per year.
This isn’t something that happens overnight. It’s the result of years of excess weight, inactivity, and genetic pressure. About 80-90% of people with type 2 diabetes have insulin resistance before they’re ever diagnosed. And for many, the first sign isn’t a blood test-it’s dark, velvety patches on the neck or armpits. That’s acanthosis nigricans, a visible marker of insulin resistance. It’s not rare. It affects up to half of obese adults with early metabolic trouble.
What Are the Real Symptoms?
Forget the myth that type 2 diabetes always comes with extreme thirst and rapid weight loss. Those happen-but only in about half the cases. The real signs are subtler, and they sneak up slowly:
- Constant fatigue-even after a full night’s sleep
- Drinking way more water than usual, then needing to pee every hour
- Feeling hungry even after eating a big meal
- Blurred vision that comes and goes
- Slow-healing cuts or frequent skin infections
- Numbness, tingling, or burning in hands or feet
- Recurrent yeast infections or urinary tract infections
Here’s the scary part: 27% of Americans with diabetes don’t even know they have it. The CDC says nearly one in four people with type 2 diabetes are undiagnosed because the symptoms feel normal. That’s why routine blood tests matter-even if you feel fine. A fasting blood sugar over 100 mg/dL or an HbA1c above 5.7% is a red flag.
Why Did This Happen to Me?
It’s not your fault. But it’s not random, either. Type 2 diabetes is a mix of genes and lifestyle-and both matter.
Genes load the gun. If you have a parent or sibling with type 2 diabetes, your risk jumps by 40%. Certain ethnic groups face higher odds: Native Americans (14.5%), African Americans (12.1%), Hispanic/Latino Americans (11.8%), and Asian Americans (9.5%) are all at greater risk than non-Hispanic White Americans (7.4%).
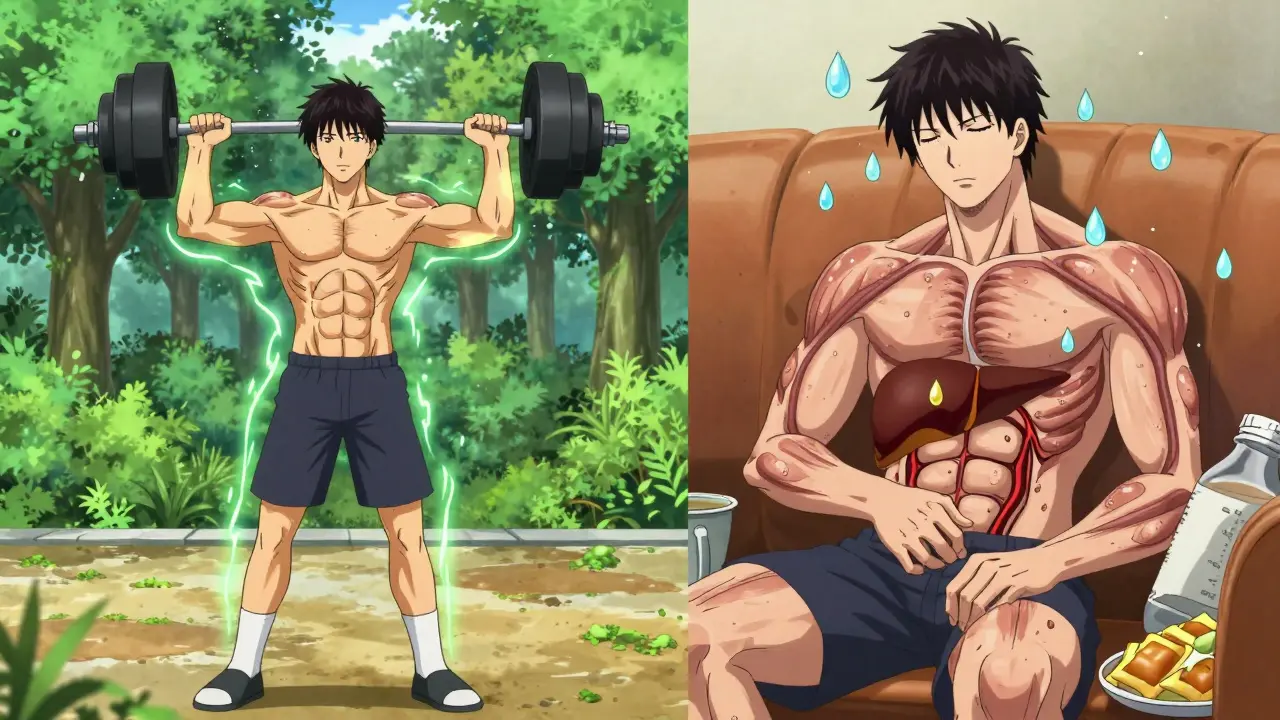
Lifestyle pulls the trigger. Obesity is the biggest driver. People with a BMI over 30 are 80 times more likely to develop type 2 diabetes than those with a BMI under 22. But it’s not just weight-it’s where the fat is stored. Belly fat, especially around the liver and pancreas, is the worst offender. Physical inactivity contributes to nearly 3 out of every 10 cases globally.
Age plays a role too. Most people are diagnosed after 45. But that’s changing. In 2022, over 287,000 Americans under 20 had type 2 diabetes-up from almost none two decades ago. Kids are developing it because of processed food, sugary drinks, and lack of movement. This isn’t just an adult problem anymore.
What Happens If You Don’t Manage It?
Left unchecked, type 2 diabetes doesn’t just stay in your blood. It damages your entire body.
- Heart and blood vessels: People with diabetes are 2 to 4 times more likely to have a heart attack or stroke. Heart disease causes 65-80% of deaths in people with type 2 diabetes.
- Nerves: After 10 years, 60-70% of people develop nerve damage. That can mean pain, numbness, or loss of feeling in the feet. And if you can’t feel a blister or cut? It turns into a foot ulcer. One in five foot ulcers leads to amputation.
- Kidneys: Type 2 diabetes causes 44% of new cases of kidney failure in the U.S. Once your kidneys start failing, you need dialysis or a transplant.
- Eyes: Diabetic retinopathy affects nearly 30% of adults with diabetes and is the leading cause of blindness in working-age adults.
- Brain: People with type 2 diabetes have a 2-3 times higher risk of Alzheimer’s. Some researchers even call it “type 3 diabetes” because insulin resistance in the brain may play a key role.
- Mental health: Depression is twice as common in people with diabetes-and it makes managing the disease harder, increasing the risk of early death by 20%.
These aren’t distant risks. They’re real outcomes-and they’re preventable.
How to Actually Manage Type 2 Diabetes
Managing type 2 diabetes isn’t about perfection. It’s about consistency. And it starts with three pillars: food, movement, and monitoring.
1. Food Is Medicine
You don’t need to go on a strict diet. You need to change your relationship with food. Focus on whole, unprocessed foods: vegetables, legumes, whole grains, lean proteins, nuts, and healthy fats. Cut out sugary drinks-that’s the single biggest dietary change you can make.
Research shows that losing just 7% of your body weight cuts your risk of developing diabetes by 58%. For someone who weighs 200 pounds, that’s 14 pounds. And it doesn’t have to happen all at once. Small, steady changes work better than drastic overhauls.
There’s also powerful evidence that some people can reverse type 2 diabetes. The DIALECT trial found that 46% of people with diabetes for less than six years went into remission after following a very low-calorie diet (825-853 calories per day for 3-5 months), followed by gradual food reintroduction. Their HbA1c dropped below 6.5%-without medication. That’s not a miracle. It’s science.
2. Move Your Body-Regularly
Exercise isn’t optional. It’s essential. Walking 30 minutes a day, five days a week, improves insulin sensitivity as much as some medications. Strength training twice a week helps too-it builds muscle, and muscle is your body’s main glucose sink.
You don’t need a gym. Take the stairs. Park farther away. Do squats while brushing your teeth. Movement adds up. And the benefits start within days.
3. Monitor Your Numbers
Know your HbA1c. That’s your average blood sugar over the past 2-3 months. Most doctors aim for under 7%. But for older adults or those with other health issues, 7-8% is safer to avoid low blood sugar episodes.
Continuous glucose monitors (CGMs) are no longer just for type 1 diabetes. In 2022, the FDA approved the first CGM for type 2 diabetes. Usage among Medicare beneficiaries jumped from 1.2% in 2017 to 12.7% in 2022. Seeing your numbers in real time helps you understand how food, stress, and sleep affect your blood sugar. That’s power.
4. Medications When Needed
Metformin is still the first-line drug. It’s cheap, safe, and reduces HbA1c by 1-2%. It also helps with weight loss and may lower heart disease risk.
But newer drugs are changing the game. GLP-1 receptor agonists (like semaglutide or tirzepatide) don’t just lower blood sugar-they help you lose weight, protect your heart, and reduce kidney damage. SGLT2 inhibitors do the same, with added benefits for heart failure and kidney protection.
These aren’t just pills. They’re disease-modifying tools. And they’re more effective than ever.

What About Remission?
Yes, type 2 diabetes can go into remission. That means your blood sugar stays normal without medication. It’s not a cure-you’re still at risk if you gain weight or stop moving. But it’s possible.
The key is early intervention. The sooner you act after diagnosis, the better your chances. Weight loss is the biggest factor. Even losing 10-15% of your body weight can put diabetes into remission for many.
And it’s not just about willpower. Structured programs like the CDC’s National Diabetes Prevention Program have helped over 100,000 people in the U.S. reduce their risk by 58% through coaching, group support, and real-life strategies.
What’s Next?
The future of type 2 diabetes care is personalized. Researchers are using AI to predict who will respond best to certain drugs. Genetic testing may soon tell you whether you’re more likely to benefit from weight loss, metformin, or a GLP-1 drug. Hybrid closed-loop systems (like the MiniMed 780G) are now available for type 2 users, automatically adjusting insulin based on real-time glucose readings.
But technology alone won’t fix this. The real challenge is access. In low-income communities, healthy food is expensive. Safe places to walk are scarce. Diabetes education is out of reach. The cost of diabetes in the U.S. is over $412 billion a year. That’s not just a medical problem-it’s a social one.
The good news? You don’t need a perfect plan to start. One healthy meal. A 10-minute walk. Checking your blood sugar once a week. These small steps add up. And they matter more than you think.
Can type 2 diabetes be reversed?
Yes, in many cases. Type 2 diabetes can go into remission-meaning blood sugar levels return to normal without medication-especially if you lose weight early after diagnosis. Studies show that losing 10-15% of body weight through structured diet and lifestyle changes can lead to remission in nearly half of people diagnosed within the last six years. It’s not a cure, but it’s a powerful outcome.
Do I need to take medication for life?
Not necessarily. Many people start with metformin, but if they lose weight, eat better, and move more, they may reduce or even stop medication. However, since type 2 diabetes is progressive, some people will eventually need more drugs or insulin over time. The goal isn’t to avoid meds forever-it’s to use them wisely and reduce dependency when possible.
Is type 2 diabetes hereditary?
Yes, genetics play a big role. If a parent or sibling has type 2 diabetes, your risk increases by about 40%. Over 400 genetic variants have been linked to the condition. But genes aren’t destiny. Even with a strong family history, lifestyle changes can delay or prevent onset by up to 60%.
What’s the best diet for type 2 diabetes?
There’s no single “best” diet, but the most effective approaches focus on whole foods: vegetables, legumes, whole grains, lean proteins, nuts, and healthy fats. Avoid added sugars, refined carbs, and ultra-processed foods. Low-carb, Mediterranean, and plant-based diets have all been shown to improve blood sugar control. The key is sustainability-pick a way of eating you can stick with long-term.
Can I still eat fruit?
Absolutely. Whole fruits contain fiber, vitamins, and antioxidants that help manage blood sugar. Apples, berries, oranges, and pears are excellent choices. Avoid fruit juices and dried fruits, which spike blood sugar quickly. One serving (like one medium apple or a cup of berries) at a time is fine for most people.
How often should I check my blood sugar?
It depends. If you’re not on insulin, checking once or twice a week might be enough to spot patterns. If you’re on medication or have trouble controlling your numbers, daily checks help. Continuous glucose monitors (CGMs) give real-time data and are becoming more common for type 2 users. Talk to your doctor about what makes sense for your situation.
Can stress make type 2 diabetes worse?
Yes. Stress triggers the release of cortisol and adrenaline, which raise blood sugar levels. Chronic stress also leads to poor sleep, emotional eating, and skipping exercise-all of which make diabetes harder to manage. Managing stress through walking, meditation, deep breathing, or therapy isn’t optional-it’s part of treatment.
What should I do if I feel dizzy or shaky?
That could be low blood sugar (hypoglycemia). If you’re on insulin or certain pills like sulfonylureas, this can happen. Eat or drink 15 grams of fast-acting sugar-like 4 ounces of juice, 3-4 glucose tablets, or 1 tablespoon of honey. Wait 15 minutes, then check your blood sugar again. If it’s still low, repeat. Always carry a source of quick sugar. Talk to your doctor if this happens often.
Where Do I Go From Here?
Start small. Pick one thing: swap soda for water. Walk 10 minutes after dinner. Write down what you eat for three days. That’s it. You don’t need to fix everything at once. Type 2 diabetes isn’t a failure-it’s a signal. And signals are meant to be listened to, not feared.
The tools are better than ever. The science is clear. The support is out there. You’re not alone. And you have more control than you think.





Shreyash Gupta
December 26, 2025 AT 19:31jesse chen
December 28, 2025 AT 07:21Ellie Stretshberry
December 29, 2025 AT 21:59Zina Constantin
December 31, 2025 AT 14:28Prasanthi Kontemukkala
January 1, 2026 AT 05:37Sarah Holmes
January 1, 2026 AT 13:04Ryan Cheng
January 1, 2026 AT 18:11Angela Spagnolo
January 1, 2026 AT 18:48Alex Ragen
January 2, 2026 AT 08:45wendy parrales fong
January 4, 2026 AT 01:41Jeanette Jeffrey
January 5, 2026 AT 10:22Dan Alatepe
January 6, 2026 AT 22:42Lori Anne Franklin
January 7, 2026 AT 15:44Jay Ara
January 7, 2026 AT 17:21