Epworth Sleepiness Scale Assessment
How often do you feel sleepy during these situations?
Rate your likelihood of dozing off in each situation (0 = Never, 1 = Seldom, 2 = Sometimes, 3 = Often)
Your Assessment Results
When you feel constantly drowsy and also rely on alcohol, pills, or other drugs, the two problems don’t just add up - they amplify each other. Understanding how sleepiness and substance abuse interact can save you from dangerous mistakes, health complications, and even life‑threatening situations.
Below you’ll learn why some substances make you nod off, why others mask tiredness, how to spot the warning signs, and what practical steps you can take to break the cycle.
Why Substances Influence Sleepiness
Sleepiness is a physiological drive to fall asleep that arises when the brain’s alertness centers are under‑stimulated. It’s regulated by the circadian rhythm, homeostatic sleep pressure, and neurotransmitters like adenosine and orexin. When you introduce a psychoactive drug, you’re essentially hijacking those same chemical pathways.
Substance Abuse describes the harmful pattern of using drugs or alcohol in a way that leads to health, social, or legal problems. Many abused substances either depress the central nervous system (CNS) or, paradoxically, keep you awake while wearing your brain down. Both outcomes increase the likelihood of unintended sleep episodes.
Common Depressants That Heighten Drowsiness
- Alcohol boosts the activity of GABA, a calming neurotransmitter, causing a rapid drop in alertness. Even a single drink can cut reaction time in half.
- Opioids bind to mu receptors, which not only dull pain but also suppress the brainstem’s arousal centers. Prescription painkillers are a leading cause of accidental drowsiness on the road.
- Benzodiazepines (e.g., diazepam, lorazepam) enhance GABA signaling, making them powerful sedatives often prescribed for anxiety or insomnia.
- Barbiturates are older sleep aids that depress the CNS more broadly and are rarely used today because of their high overdose risk.
These drugs share a common thread: they lower the brain’s excitation threshold, making it easier for the natural sleep drive to win.
Stimulants That Mask Sleepiness - The Hidden Danger
People sometimes turn to caffeine, nicotine, or prescription stimulants like Adderall to stay awake while they’re actually sleep‑deprived. The short‑term boost can feel great, but the underlying sleep pressure doesn’t disappear. When the stimulant wears off, the crash can be more severe than the original drowsiness.
Repeated cycles of “fuel‑up‑then‑crash” erode sleep architecture, reduce REM sleep, and increase the risk of chronic fatigue, mood swings, and even substance dependence.
Recognizing the Warning Signs
There are clear behavioral and physiological cues that point to a dangerous combination of sleepiness and substance use:
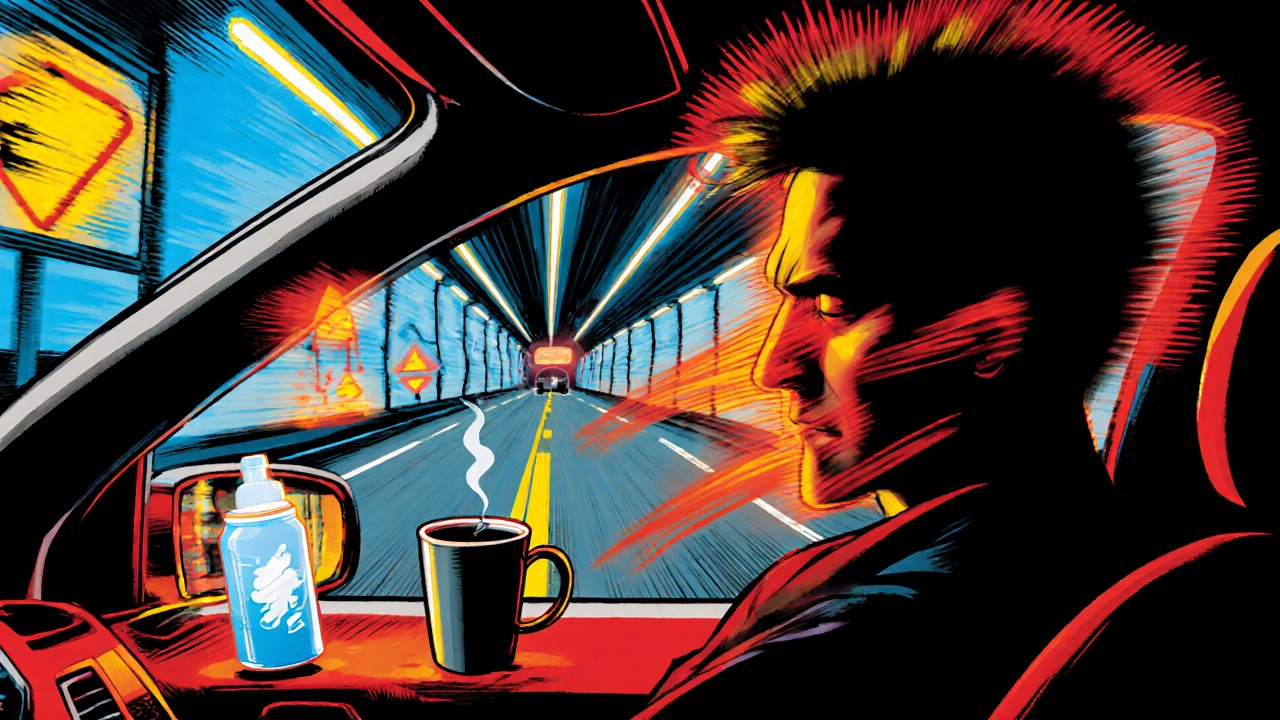
- Microsleeps - brief, involuntary dozes lasting a few seconds, often while driving or working.
- Frequent yawning, heavy eyelids, or difficulty keeping eyes open.
- Reliance on “pick‑me‑ups” (energy drinks, extra coffee) to function.
- Blackouts or memory gaps after drinking or using opioids.
- Increased tolerance - needing more of a drug just to feel its usual effect.
One quick screening tool is the Epworth Sleepiness Scale, a questionnaire that scores your likelihood of dozing off in everyday situations. A score above 10 usually signals excessive daytime sleepiness and warrants professional evaluation.
Health Risks of the Combined Behaviors
When drowsiness meets drug impairment, the consequences extend beyond simple fatigue:
- Accidents: Drowsy driving combined with alcohol is up to five times more likely to result in a crash than either factor alone.
- Mental health decline: Chronic sleep loss worsens anxiety and depression, which in turn can fuel further substance use - a vicious feedback loop.
- Cardiovascular strain: Both sleep deprivation and certain drugs raise blood pressure and heart rate, increasing the risk of heart attack or stroke.
- Immune suppression: Poor sleep reduces natural killer cell activity; combining it with opioids further impairs immune response, making infections more common.
Even conditions like Narcolepsy - a neurological disorder characterized by sudden sleep attacks - can be misdiagnosed when substance use is the primary focus. Proper assessment is essential.
Getting Help: Treatment Options That Address Both Issues
Effective programs treat the sleep problem and the substance use simultaneously. Here are the most widely available approaches:
- Medication‑assisted treatment (MAT): Combines FDA‑approved medications (e.g., buprenorphine for opioid dependence) with counseling. Some MAT protocols also incorporate low‑dose sleep‑promoting agents for those with co‑occurring insomnia.
- Cognitive Behavioral Therapy for Insomnia (CBT‑I): A short‑term, evidence‑based program that restructures thoughts and habits around sleep. It reduces reliance on hypnotics and improves daytime alertness.
- Integrated dual‑diagnosis programs: Specialized clinics assess both mental health/substance use and sleep disorders, creating a unified care plan.
- Support groups: 12‑step meetings, SMART Recovery, and peer‑led sleep‑health groups provide accountability and shared strategies.
- Lifestyle coaching: Sleep hygiene education (consistent bedtime, dark room, limited screen time) paired with harm‑reduction advice (e.g., limiting alcohol to weekends) can stabilize both domains.
When you reach out, be ready to share a brief timeline of your sleep patterns, substance use frequency, and any past treatment attempts. The more data you give, the faster a clinician can match you with the right program.
Prevention Tips You Can Start Today
- Set a regular sleep‑wake schedule - even on weekends - to reinforce your circadian rhythm.
- Limit alcohol to one standard drink per day and avoid it before bedtime.
- Use stimulants sparingly. If you need a caffeine boost, keep it under 200mg and stop after 2p.m.
- Track your daytime alertness with a simple journal or a phone app; note any instances of microsleep.
- Seek early professional help if you notice the warning signs repeatedly. Early intervention cuts the risk of chronic dependence.
Remember, improving sleep quality often reduces cravings for depressants, and cutting back on substances can make sleep feel more natural.

Quick Reference Checklist
- Assess daytime sleepiness with the Epworth Sleepiness Scale.
- Identify substances you use and their typical impact on alertness.
- Look for red flags: microsleeps, blackouts, increased tolerance.
- Choose a treatment path: MAT, CBT‑I, integrated dual‑diagnosis, or support groups.
- Implement sleep hygiene: fixed schedule, dark environment, limited caffeine/alcohol.
Frequently Asked Questions
Can occasional drinking cause dangerous drowsiness?
Yes. Even a few drinks can impair the brain's arousal system, making you feel sleepy faster than if you hadn't had any alcohol. The effect is stronger if you’re already sleep‑deprived.
Is it safe to use caffeine to stay awake while I’m recovering from opioid use?
Caffeine can help offset temporary fatigue, but it won’t replace the restorative function of sleep. Over‑reliance may worsen anxiety and interfere with MAT protocols. Use it modestly and focus on rebuilding healthy sleep patterns.
What is the best way to know if I have a sleep disorder underlying my drowsiness?
Start with a sleep diary and the Epworth Sleepiness Scale. If scores remain high, schedule a polysomnography (sleep study) or a consultation with a sleep specialist. They can rule out narcolepsy, sleep apnea, or restless‑leg syndrome.
Do support groups help with both sleep problems and substance use?
Many peer‑led groups now include sleep‑health modules. Sharing strategies for better sleep hygiene alongside recovery stories creates a supportive environment that tackles both issues together.
How long does it usually take to feel better after stopping depressant use?
Recovery timelines vary. Acute withdrawal may last 1‑2 weeks, but sleep patterns often stay disrupted for a month or more. Engaging in CBT‑I and maintaining a consistent routine can speed up the normalization of sleep.
Putting It All Together
If you’ve recognized that excessive sleepiness and substance use are tangled in your life, the first step is to break the cycle with awareness. Use the checklist, talk to a health professional, and choose a treatment that addresses both sleep and addiction. Small, consistent changes in bedtime habits, substance moderation, and seeking support can restore alertness, safety, and overall wellbeing.






Daisy canales
October 16, 2025 AT 16:56Wow, because we all love mixing booze with nap time, right?
keyul prajapati
October 17, 2025 AT 20:42It is essential to recognize that the neurochemical pathways governing wakefulness and sedation are not independent entities but rather form a tightly interwoven network. When a depressant such as alcohol or an opioid engages the GABAergic system, it reduces neuronal firing rates dramatically, which in turn lowers the threshold for the brain’s intrinsic sleep drive. Conversely, stimulants like caffeine or prescription amphetamines elevate catecholamine levels, temporarily boosting alertness but also masking the accumulation of homeostatic sleep pressure. Over time, this push‑pull dynamic can lead to a state where micro‑sleep episodes punctuate periods of intense focus, especially during tasks that demand sustained attention, such as driving or operating machinery. The resultant microsleeps are often unnoticed by the individual yet pose a catastrophic risk to public safety. Moreover, the repeated cycling between sedation and artificial arousal deteriorates the architecture of REM sleep, undermining memory consolidation and emotional regulation. This degradation can exacerbate underlying mood disorders, creating a vicious feedback loop that fuels further substance use as a maladaptive coping mechanism. From a physiological perspective, the hypothalamic orexin system, which normally stabilizes wakefulness, becomes dysregulated under chronic substance exposure, further compromising the ability to stay awake without external pharmacological support. In practice, clinicians should assess not only the quantity of substance consumed but also the timing relative to the individual’s circadian rhythm, as night‑time use of depressants aligns poorly with natural melatonin peaks. Screening tools such as the Epworth Sleepiness Scale provide a quantitative measure of daytime somnolence and can flag individuals who are at heightened risk for accidents. Intervention strategies that combine Medication‑Assisted Treatment (MAT) with Cognitive Behavioral Therapy for Insomnia (CBT‑I) have demonstrated efficacy in simultaneously addressing both domains. Lifestyle modifications, including strict sleep‑hygiene practices and limiting alcohol intake to low‑risk thresholds, are indispensable components of a comprehensive treatment plan. Finally, it is critical to destigmatize the co‑occurrence of sleep disorders and substance use disorders, encouraging patients to seek integrated care rather than compartmentalized services.
Alice L
October 19, 2025 AT 00:29Esteemed members of the community, I wish to convey my sincere appreciation for the thorough exposition presented herein. The synthesis of neurophysiological mechanisms with pragmatic guidance is commendable, and I would like to underscore the paramount importance of culturally sensitive approaches when addressing such intertwined health concerns. Respectful acknowledgment of diverse lived experiences augments the efficacy of therapeutic interventions.
Seth Angel Chi
October 20, 2025 AT 04:16While the prior comment is earnest it overlooks the fact that not all readers have access to integrated clinics; many are left navigating fragmented care.
Kristen Ariies
October 21, 2025 AT 08:02Absolutely love how this post breaks down the science-let's take action! 💪
First, set a bedtime alarm tomorrow!
Second, swap that night‑cap for a calming tea!
Third, join a local support group and share your progress!
Remember, consistency is the key, and every small win builds momentum! You’ve got this!!!
Donny Bryant
October 22, 2025 AT 11:49Great info! I think just keeping a simple sleep diary can really help you see patterns. Try noting when you drink or take meds and how you feel the next day. It’s a quick way to start making changes.
kuldeep jangra
October 23, 2025 AT 15:36I completely agree with the suggestion to keep a diary; it provides a concrete record that can be shared with clinicians, which often accelerates the tailoring of treatment strategies. In addition, consider pairing the diary with a brief daily gratitude note; this practice can improve mood and reduce reliance on substances as a coping mechanism. Moreover, try to establish a wind‑down routine that includes dim lighting, a brief stretch, and perhaps a short meditation session; these activities train your brain to associate certain cues with sleep readiness. If you notice persistent cravings during the evening, it may be helpful to have a list of alternative activities-such as reading a chapter of a novel, working on a puzzle, or engaging in light journaling-so that the urge to reach for a drink or pill is met with a healthier option. Lastly, stay connected with peers who are also on a recovery path; sharing successes and setbacks in a supportive environment can reinforce commitment and provide fresh ideas for managing sleep‑related challenges.
harry wheeler
October 24, 2025 AT 19:22Remember the diary can be digital as well you can sync it with a sleep app for better insights
faith long
October 25, 2025 AT 23:09I hear you loud and clear-this stuff is not just "nice to know" it’s a matter of survival. When you’re waking up at 3 am feeling your heart race because you chugged another coffee to outrun a hangover, you’re literally fighting a war inside your skull. That desperation breeds aggression, and you end up lashing out at anyone who tries to point out the obvious: you’re stuck in a vicious cycle. So stop the self‑pity, grab that diary, and start carving out a real path out of this mess before it devours you completely.
Samantha Dean
October 27, 2025 AT 01:56In pondering the intricate nexus between somnolence and psychoactive consumption, one is reminded of the ancient Maxim that health is the harmony of body and mind. To neglect either facet is to invite discord, which inevitably manifests in diminished cognition and compromised wellbeing.
Vanessa Peters
October 28, 2025 AT 05:42The analysis presented earlier, while thorough, fails to capture the sheer drama of daily human struggle-a chaotic ballet where each misstep can be fatal. The stakes are high, and the data alone cannot soothe the panic that courses through a fatigued mind.
Suzan Graafstra
October 29, 2025 AT 09:29Ah, the human condition-ever teetering between the abyss of exhaustion and the seductive glow of chemical escape. We are but actors on a stage, our scripts written in the ink of sleepless nights and fleeting highs.
Ralph Louis
October 30, 2025 AT 13:16Yo, if you think you can just sprinkle a few tips and be golden, think again. The real world is messy, people are lazy, and most of us ain’t gonna follow some checklist while buzzed.
Harshitha Uppada
October 31, 2025 AT 17:02lol you sound like a bored highschooler spitting out random advice; reality is you cant fix deep rooted stuff with simple rules...