Steroid-Induced Hyperglycemia Insulin Calculator
Adjust Insulin for Steroid Therapy
Calculate the additional insulin needed when taking steroids. Based on clinical guidelines for safe steroid-induced hyperglycemia management.
Adjusted Insulin Plan
Key Guidelines Applied
• Baseline: 0.1 U/kg
• Prednisone: NPH morning dose
• Dexamethasone: Long-acting analogues
• Correction doses: 0.04-0.08 U/kg for high BG
- For prednisone, use NPH insulin in the morning
- For dexamethasone, use glargine or detemir
- Adjust insulin as steroid dose decreases
- Monitor blood sugar 4x daily during therapy
For continuous background coverage
For mealtime and correction doses
Critical Safety Note
Do not adjust insulin without medical supervision. This calculator provides guideline-based estimates only. Always consult your healthcare provider before changing insulin regimens. Never reduce insulin too slowly during steroid tapering to avoid dangerous low blood sugar.
When you start taking steroids like prednisone or dexamethasone, your blood sugar can spike-sometimes dramatically. This isn’t just a side effect. It’s a predictable, well-documented metabolic shift called steroid-induced hyperglycemia. For people with diabetes, this can turn an already tricky condition into a daily balancing act. For those without diabetes, it might be the first sign they’re at risk. The key isn’t to avoid steroids when they’re medically necessary. It’s to adjust your diabetes medications correctly so you don’t end up in the hospital from high blood sugar… or worse, from a crash when the steroid dose drops.
Why Steroids Raise Blood Sugar
Steroids don’t just reduce inflammation-they mess with how your body uses insulin. They make your liver pump out more glucose, even when you don’t need it. They block insulin from doing its job in your muscles and fat. And over time, they dull the pancreas’s ability to produce insulin when it’s needed. This combination creates a perfect storm: too much glucose in, not enough insulin to handle it. The timing matters. Blood sugar usually starts climbing 4 to 8 hours after you take a steroid dose. It peaks around 24 hours later. That means if you take prednisone in the morning, your sugar will likely spike by lunchtime and stay high through the evening. If you’re on dexamethasone, which lasts longer, the spike can drag on for two or three days. This isn’t random. It’s pharmacology.Who’s at Risk
About 40% of hospitalized patients on steroids develop high blood sugar. That number jumps to 50% if you already have diabetes. Type 1 diabetes patients often need bigger insulin increases-30% to 50%-than those with type 2, who typically need 20% to 30%. But even people without prior diabetes can go from normal to diabetic-range sugars in just a few days of steroid treatment. The dose makes a difference. A 5-day course of 10 mg prednisone might cause a mild rise. But 40 mg or more? That’s a major metabolic stress test. And it’s not just the dose-it’s the type. Dexamethasone lasts longer than prednisone, so its effects are more prolonged. That means your insulin plan needs to match that timing.Insulin: The First-Line Tool
For most patients, especially in hospitals or with severe hyperglycemia, insulin is the go-to. Oral meds like metformin or GLP-1 agonists can help in mild cases, but insulin gives you the control you need when steroids are doing their worst. Start with a baseline: 0.1 unit of insulin per kilogram of body weight. So if you weigh 70 kg, that’s about 7 units total. Split it between basal (background) and bolus (mealtime) insulin. But here’s the catch: don’t just copy your usual dose. Add to it. For prednisone, use NPH insulin in the morning. Its 12-36 hour duration lines up with prednisone’s 18-36 hour half-life. For dexamethasone, use glargine or detemir-long-acting insulins that cover the 36-72 hour window. Giving NPH at night for dexamethasone? That’s a recipe for missing the peak. Correction doses matter too. If your blood sugar hits 11.1-16.7 mmol/L (200-300 mg/dL), give 0.04 units per kg. If it’s above 16.7 mmol/L, give 0.08 units per kg. These aren’t guesses. They’re evidence-backed numbers from clinical guidelines.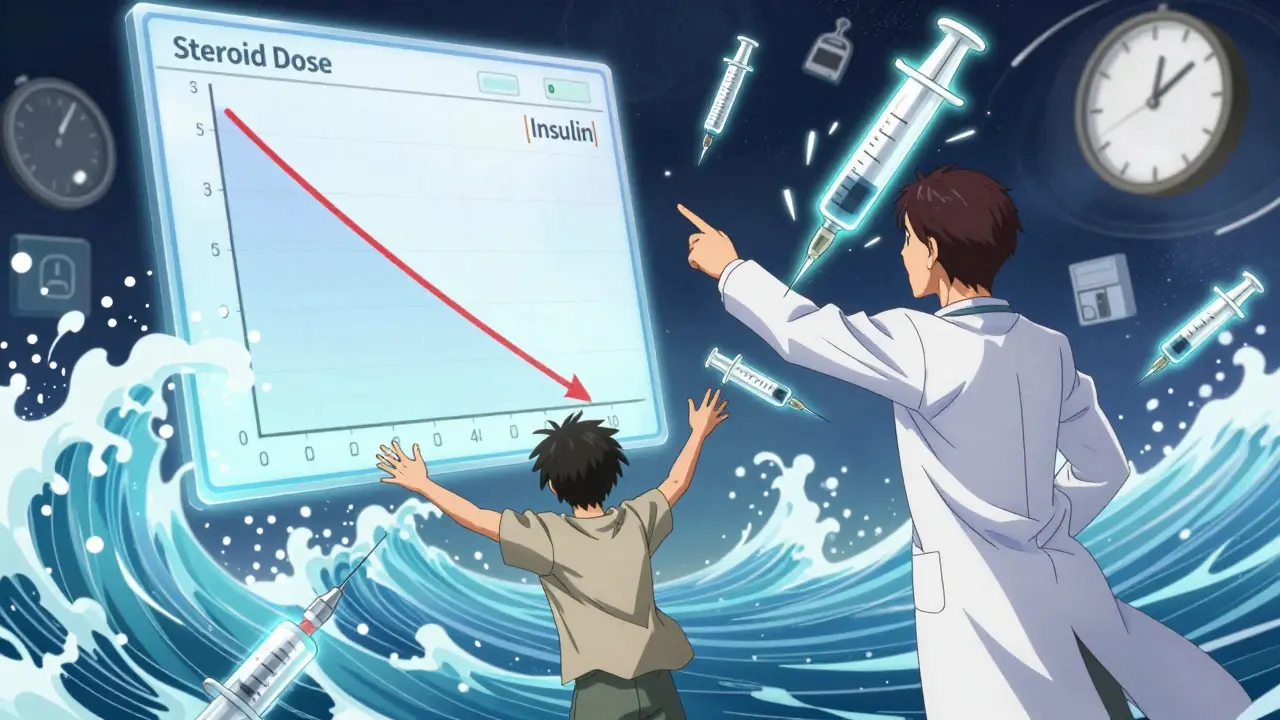
Monitoring: More Than Just Fingersticks
Check your blood sugar at least four times a day: before meals and at bedtime. But if your steroid dose changes, or your sugar is running high, check every 2-4 hours. Don’t wait until you feel bad. Continuous glucose monitors (CGMs) are game-changers. They show you trends-not just snapshots. You can see when your sugar climbs after your steroid dose and how long it stays high. The goal? Spend at least 70% of your day between 3.9 and 10.0 mmol/L. Less than 4% of your time should be below 3.9 mmol/L. That’s the sweet spot. If you’re on an insulin pump, you might need to raise your basal rate by 25-50% during the peak steroid effect. But when the steroid drops, you have to drop it back fast-or risk a low.The Tapering Trap
This is where most people get hurt. Steroid-induced hyperglycemia doesn’t vanish the day you stop taking steroids. It fades slowly-over 3 to 4 days. But insulin doesn’t. If you keep your full dose, your blood sugar will crash. That’s not a myth. It’s a real risk. A 2021 study at Johns Hopkins found 27% of patients on sulfonylureas (like glipizide) had emergency visits for low blood sugar during steroid tapering. Insulin users had fewer issues-but only if their doses were lowered in sync with the steroid. Here’s how to avoid it: reduce insulin as you reduce steroids. If you were on 40 mg prednisone and needed 50% more insulin, and now you’re down to 20 mg, cut your insulin back by 20-30% immediately. Don’t wait. Don’t assume your doctor will do it. Track your sugar. Adjust. One patient on Reddit said it best: “When I dropped from 40mg to 20mg of prednisone, my endocrinologist didn’t reduce my insulin fast enough. I had three hypos in two days.” That’s preventable.What About Oral Medications?
Metformin can help in mild cases, especially for outpatients. It reduces liver glucose output-exactly what steroids overwork. GLP-1 agonists and DPP-4 inhibitors are also options, but they’re slower to act. They’re not ideal when you need fast, precise control. Sulfonylureas? Avoid them during steroid therapy. They force your pancreas to keep pumping out insulin. When the steroid tapers, your pancreas keeps going-and your blood sugar plummets. That’s why insulin is safer. You control the dose. You can turn it down.
Practical Tips for Daily Life
- Plan ahead. If you know you’re getting steroids, talk to your diabetes team before you start. Get a plan written down. - Match insulin to steroid timing. Morning steroid? Morning insulin. Evening steroid? Adjust accordingly. Don’t assume one-size-fits-all. - Keep a log. Write down your steroid dose, insulin dose, and blood sugar readings. Patterns emerge. - Use CGM alerts. Set alerts for highs and lows. Don’t rely on how you feel. - Don’t panic over one high reading. Wait 24 hours after a steroid dose before making big changes. The peak isn’t immediate. - Know your taper schedule. If your doctor cuts your steroid dose on Tuesday, expect your insulin needs to drop by Thursday or Friday.What Happens After Steroids?
Once the steroid is fully off, your blood sugar should return to baseline within a week. But not always. Some people develop permanent insulin resistance. Others, especially those with prediabetes, may never go back to normal. That’s why follow-up testing matters. Check your HbA1c in 3 months. If it’s elevated, you may need ongoing treatment.Bottom Line
Steroid-induced hyperglycemia is common. It’s dangerous. But it’s manageable. The biggest mistake isn’t failing to treat high blood sugar-it’s failing to reduce insulin when the steroid does. You need to be proactive, precise, and patient. Track your numbers. Adjust your meds. And never assume your doctor will do it for you.Can steroids cause diabetes in people who don’t have it?
Yes. Steroid-induced hyperglycemia can push someone with prediabetes into full-blown diabetes, especially with long-term or high-dose use. About 10-15% of people without prior diabetes develop persistent high blood sugar after prolonged steroid therapy. Screening with HbA1c or fasting glucose 3 months after stopping steroids is recommended.
Should I stop my diabetes meds if my sugar is normal while on steroids?
No. Even if your sugar looks normal, steroids are still working in your body. Stopping your meds can lead to a dangerous rebound spike later. Always adjust under medical guidance, not based on a single reading.
Is it safe to use metformin with steroids?
Yes, for mild cases. Metformin helps reduce liver glucose production, which steroids overstimulate. It’s often used alongside insulin or as a standalone for outpatients with modest sugar spikes. But if your blood sugar is above 16.7 mmol/L, insulin is more effective and faster-acting.
Why is NPH insulin recommended for prednisone but not dexamethasone?
Prednisone lasts 18-36 hours, and NPH insulin peaks at 4-12 hours and lasts up to 36 hours-so they align well. Dexamethasone lasts 36-72 hours. NPH’s peak doesn’t cover the full duration, leading to gaps in control. Long-acting analogues like glargine provide steady coverage without peaks, matching dexamethasone’s prolonged effect.
How soon should I reduce insulin after stopping steroids?
Start reducing insulin 3-4 days after your last steroid dose. The hyperglycemic effect fades slowly, and insulin doesn’t. If you cut your steroid dose on Monday, begin reducing insulin by Friday. Monitor closely-reducing too fast can cause hypoglycemia, but not reducing enough can cause lows too.
Can I use an insulin pump during steroid therapy?
Yes, and it’s often ideal. You can increase your basal rate by 25-50% during peak steroid effect and reduce it as the steroid tapers. But you must monitor closely. Pump users are at higher risk of rapid lows if insulin isn’t adjusted in time during tapering. Always have fast-acting carbs on hand.
What if I’m on oral meds and my doctor wants to start insulin?
It’s not a failure-it’s smart management. Oral meds can’t keep up with the speed and severity of steroid-induced spikes. Insulin gives you direct control. Many patients switch temporarily and go back to pills after steroids end. There’s no shame in using the right tool for the job.





Henry Ip
January 15, 2026 AT 13:03Just got off prednisone after 3 weeks and this post nailed it. My sugar was hitting 280 every afternoon even though I was eating clean. Started NPH at 7am like they said and boom-stable by noon. No more panic attacks before dinner.
Also learned the hard way: don’t trust how you feel. Felt fine at 220. Ended up in the ER.
CGM saved my life.
Kasey Summerer
January 16, 2026 AT 04:28So steroids turn you into a diabetic for a few weeks? Cool. Guess I’ll just start calling my pancreas ‘the traitor’ and move on.
Meanwhile my endo is still using a slide rule and thinks ‘check it once a day’ is a solid plan 😅
kanchan tiwari
January 18, 2026 AT 01:12THEY KNOW. THEY ALL KNOW. Why do you think they push steroids so hard? It’s not about inflammation-it’s about testing how many people they can turn into diabetics before we wake up. Big Pharma’s new profit model: make you sick, then sell you insulin for life. I saw the memo. They’re calling it ‘Metabolic Re-Programming.’
Don’t let them gaslight you. Your body is fighting back. I’m off all meds. Only lemon water and crystals now. 💎🫖
Bobbi-Marie Nova
January 19, 2026 AT 10:17Okay but can we talk about how no one tells you this stuff before you start steroids? I thought ‘side effects’ meant weight gain and acne. Not ‘your pancreas just quit its job.’
Also-yes, CGM is magic. I set a 200 alert and now I nap like a champ instead of panicking at 3am. Also, my cat judges me less now. Win-win.
Also also-don’t be like me and try to ‘tough it out’ with metformin alone. I cried into my glucose monitor. It was messy.
Insulin is not weakness. It’s just… better math.
Allen Davidson
January 21, 2026 AT 06:38People keep saying ‘talk to your doctor’ like that’s a solution. My endo didn’t even know NPH was better for prednisone. I had to send him the Johns Hopkins paper. He said ‘interesting’ and didn’t change my dose for 48 hours.
Stop waiting for permission. Track your numbers. Adjust. If your doc won’t help, find one who will. Your life isn’t a waiting room.
Also-yes, insulin tapering is a silent killer. I saw a guy crash after his last dose. He didn’t even know why. Don’t be him.
Rob Deneke
January 23, 2026 AT 03:41Use insulin when you need it dont be scared of it
My sugar went from 120 to 310 on 20mg prednisone
Added 6 units basal and 4 units before meals
Now I’m at 140
Stop overthinking it
Just do the math
And write it down
Trust the numbers not your gut
My gut told me to skip insulin once
Bad idea
So bad
Now I log everything
Even my coffee
Because caffeine lies
Riya Katyal
January 25, 2026 AT 02:43Oh so now I’m supposed to be a diabetic scientist just because I took a pill for my back? Thanks for the 3000-word essay, but I’m just trying to get through the week without fainting.
Also-why does everyone assume I have a CGM? I’m on Medicaid. My glucose meter has one button.
And yes, I know I should’ve planned ahead. But my doctor said ‘it’s just a short course’ and then I got extended for 6 weeks.
So no, I don’t have a plan. I have anxiety and a phone full of screenshots of my sugar spikes.
Thanks for the info. Now I feel worse.
waneta rozwan
January 25, 2026 AT 09:53This is why I stopped trusting doctors. You think you’re getting help, but really you’re just becoming a walking lab rat.
They give you steroids. They don’t warn you. Then they act shocked when you crash.
And now they want you to ‘adjust’ your insulin like you’re a robot?
What if you don’t have the time? The money? The energy?
And what if you’re just a single mom working two jobs and your kid’s school calls because you passed out in the parking lot?
This isn’t ‘manageable.’ It’s a system failure.
And you’re all just giving tips like it’s a cooking show.
Where’s the accountability?
Where’s the change?
Why do we keep pretending this is just a ‘personal responsibility’ issue?
Nicholas Gabriel
January 27, 2026 AT 06:32Important note: if you’re on insulin and your steroid dose drops, reduce your basal insulin by 10-15% every 24 hours after the last steroid dose-not all at once. I learned this the hard way after a 4am hypo that required my neighbor to call 911. Also, keep glucagon on hand. Even if you think you’re fine. Trust me. The crash doesn’t wait for business hours. And if you’re using an insulin pump, don’t forget to reset your correction factor after tapering. It’s easy to forget. I did. Twice. You’re not alone. We’ve all been there. Just be gentle with yourself. This is hard. But you’re doing better than you think.
swarnima singh
January 28, 2026 AT 13:46you know what they dont tell you? the guilt. when you go low after the steroids stop and you think ‘did i do this to myself?’ like you failed your body. but its not your fault. its the system. the meds. the timing. the silence. i cried for 3 days after my first hypo. not because of the sugar. because i thought i was broken. turns out i was just human. and the system forgot to tell me how to survive.
Isabella Reid
January 30, 2026 AT 04:24One sentence: if your doctor doesn’t know the difference between NPH and glargine for steroid timing, find a new one.
Also-yes, you can still have pizza. Just adjust. And yes, it’s okay to hate this. But you’re still winning.