When a patient walks in with shortness of breath, fatigue, or swollen ankles, the question isn’t just what’s wrong-it’s how fast can you rule out heart failure? In emergency rooms and outpatient clinics across Australia and beyond, the answer often starts with a simple blood test: NT-proBNP.
Why NT-proBNP Matters More Than Ever
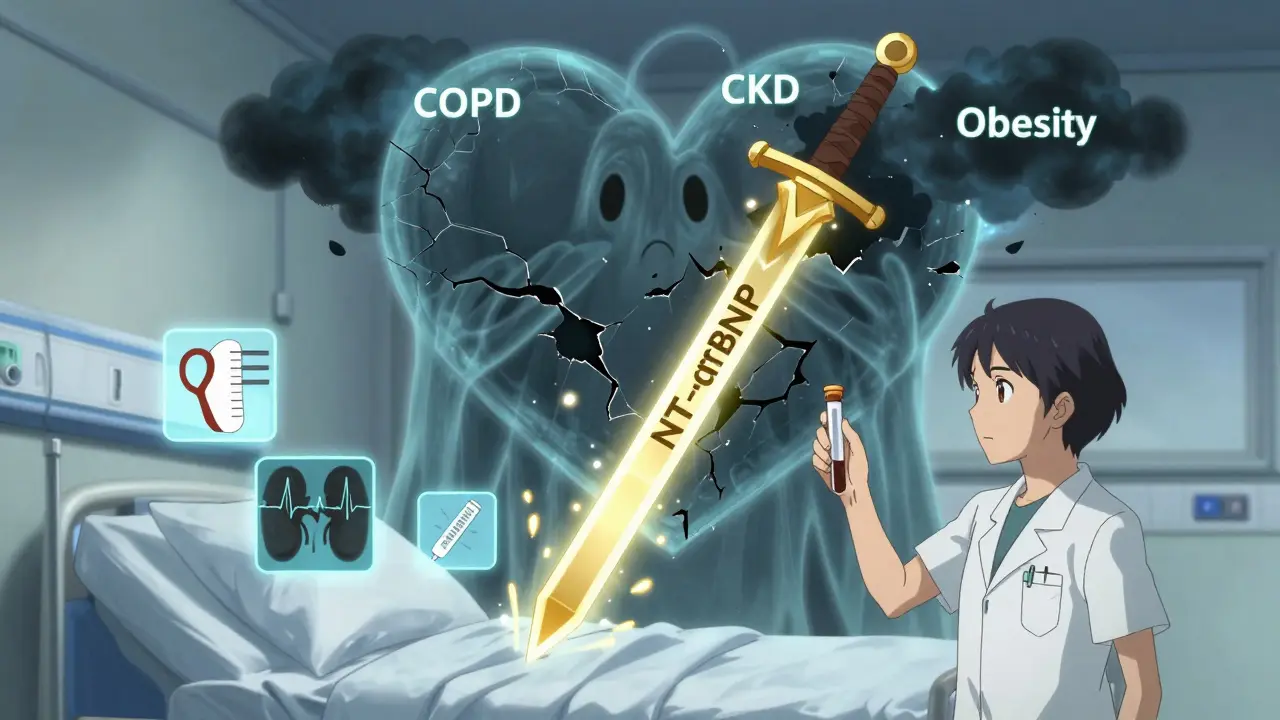
NT-proBNP, or N-terminal pro-B-type natriuretic peptide, isn’t just another lab order. It’s a direct signal from the heart telling you whether it’s under strain. When the heart’s ventricles stretch from too much pressure or fluid, they release this protein fragment into the bloodstream. The higher the level, the more likely heart failure is driving the symptoms. Unlike older methods that relied on chest X-rays or guesswork, NT-proBNP gives you a number you can trust. A level below 300 pg/mL almost always means heart failure isn’t the cause-98% of the time. That’s powerful. It means you can avoid unnecessary hospital admissions, skip expensive echocardiograms, and focus on other causes like COPD flare-ups, kidney issues, or even anxiety. This isn’t theory. In the UK, after NICE guidelines pushed NT-proBNP into emergency departments, unnecessary echocardiograms dropped by 19%. In U.S. hospitals, 89% of cardiologists now call it essential. And with point-of-care machines delivering results in under 12 minutes, you’re no longer waiting hours for an answer.When to Order It: The Clear Clinical Triggers
You don’t order NT-proBNP for every patient with a cough. You order it when the clinical picture suggests heart failure is possible-and you need to rule it in or out fast.- Acute dyspnea in patients over 50, especially with risk factors like hypertension, diabetes, or prior heart attack.
- New-onset fatigue or reduced exercise tolerance in older adults, where symptoms are vague but concerning.
- Unexplained peripheral edema without clear liver, kidney, or venous causes.
- Patients with known heart disease who develop worsening symptoms-this helps distinguish decompensation from other issues.
- Post-acute coronary syndrome, where elevated NT-proBNP predicts higher risk of death or rehospitalization.
How to Interpret the Numbers-It’s Not Just One Cut-Off
Here’s where things get real. NT-proBNP levels rise naturally with age. A level of 600 pg/mL might be normal for an 80-year-old but alarming for a 45-year-old.- Under 50 years: Rule-out threshold is < 450 pg/mL
- 50-75 years: Rule-out threshold is < 900 pg/mL
- Over 75 years: Rule-out threshold is < 1,800 pg/mL
What NT-proBNP Won’t Tell You (And What You Need to Do Instead)
This test is a gatekeeper, not a crystal ball. A high result doesn’t tell you if it’s systolic failure, diastolic failure, or just atrial fibrillation. It doesn’t tell you if the patient needs a diuretic, an ACE inhibitor, or a pacemaker. That’s why you never use it alone. Always pair it with:- Physical exam (jugular venous pressure, lung crackles, peripheral edema)
- ECG (for arrhythmias, ischemia, or left ventricular hypertrophy)
- Chest X-ray (if fluid overload is suspected)
- Renal function and electrolytes (to assess kidney impact and guide diuretic use)
Practical Tips for Ordering and Avoiding Pitfalls
Many clinicians order NT-proBNP too early or too often. Here’s how to get it right:- Order it once at initial presentation. Repeat testing only if symptoms change or you’re monitoring treatment response.
- Use serum samples, not plasma. The test requires serum separator tubes.
- Store properly: Stable for 72 hours at 4°C, or up to 6 months frozen at -70°C. Don’t let samples sit in the phlebotomy room overnight.
- Don’t test asymptomatic patients. Medicare data shows 18% of tests are ordered without symptoms-this drives up costs and causes false alarms.
- Know your lab’s reference range. Different assays (Roche, Siemens) can vary slightly. Always check local norms.
What’s Changing in 2025 and Beyond
The landscape is evolving. Starting January 2025, Medicare in the U.S. will require prior authorization for NT-proBNP tests in asymptomatic patients. That’s a sign the system is pushing back against overuse. New guidelines due in late 2024 will expand its role to include risk prediction after heart attacks. The VICTORIA trial showed that patients with falling NT-proBNP levels after an acute event had 35% lower risk of death. That’s changing how we think about recovery. Point-of-care devices like the Roche Cobas h 232 are now in use in rural clinics and ambulances. Results in 12 minutes mean you can make decisions before the patient even reaches the hospital. But the core hasn’t changed. NT-proBNP remains the most validated, reliable, and cost-effective biomarker for heart failure in clinical practice. With 28 years of outcome data backing it, it’s not going anywhere.Real Cases, Real Impact
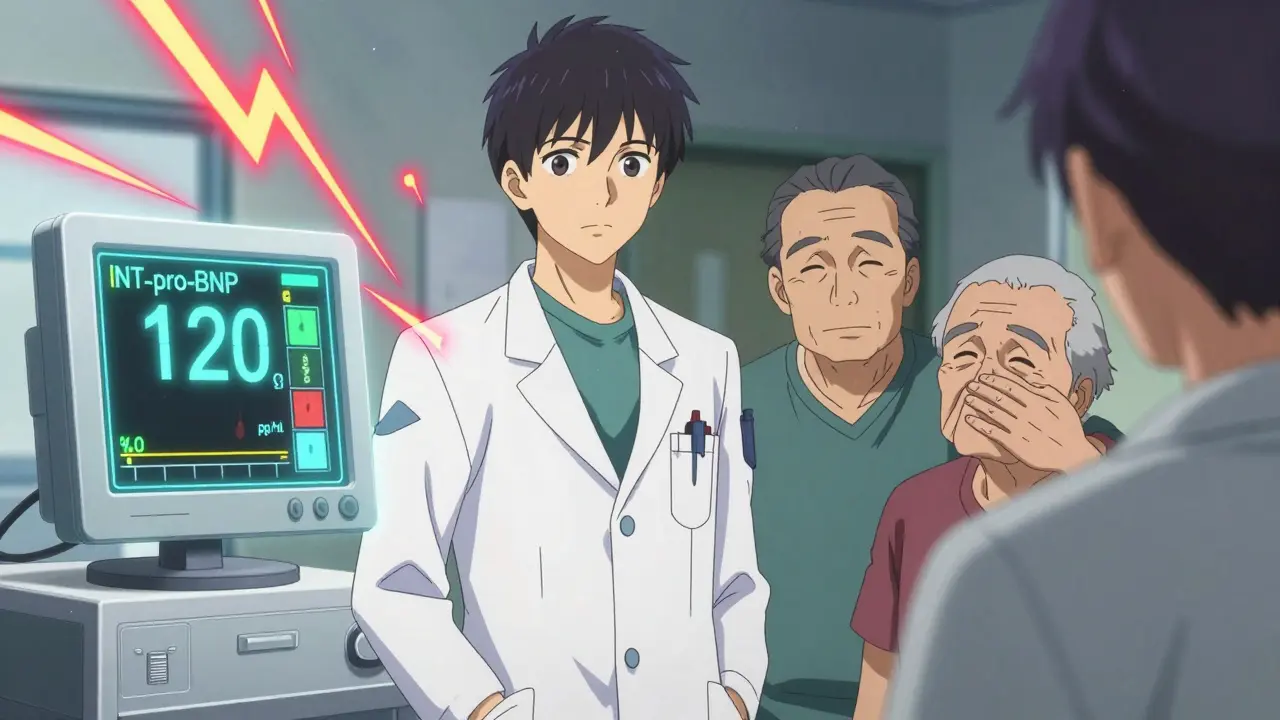
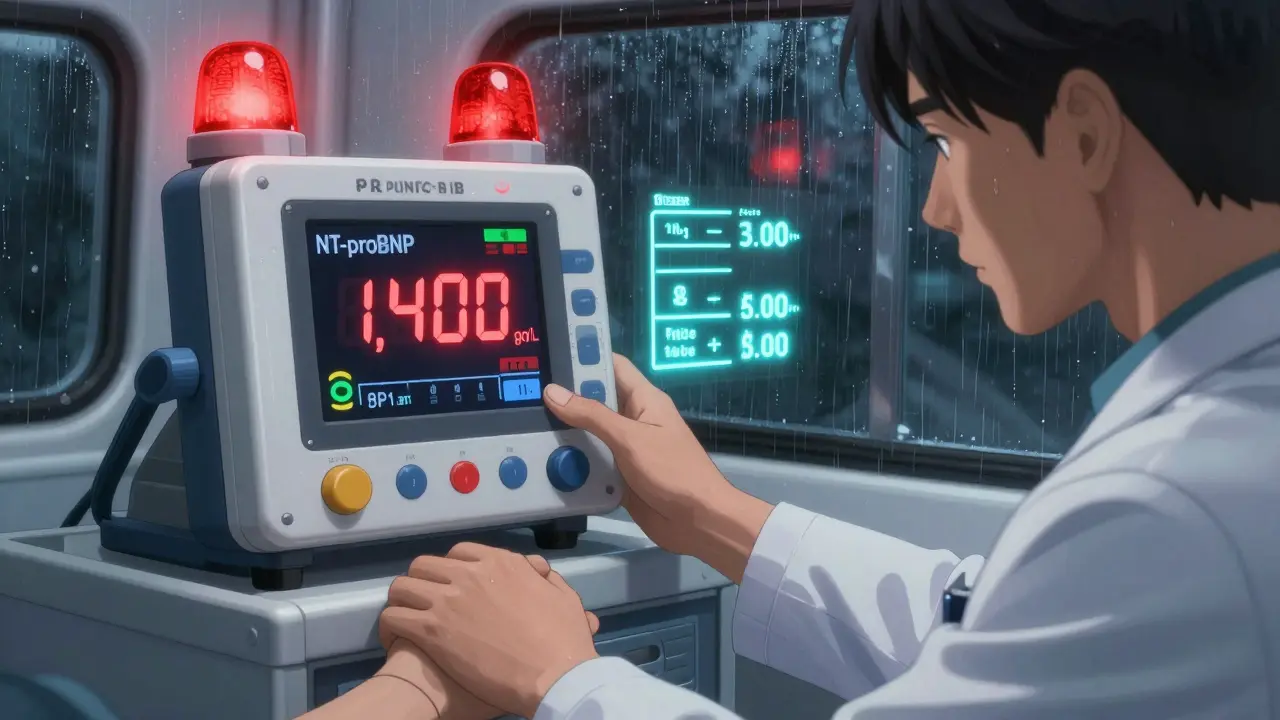
One cardiologist in Melbourne shared a story: an 82-year-old woman came in with worsening breathlessness. She had COPD, was on home oxygen, and her GP ordered an echo. The cardiologist ordered NT-proBNP instead. Result: 120 pg/mL. No heart failure. The patient had a COPD flare. The echo was canceled. Saved $3,000. Avoided unnecessary sedation and stress. Another case: a 70-year-old man with diabetes and CKD had an NT-proBNP of 1,400 pg/mL. He was tired. Swollen legs. The team almost started diuretics. But after reviewing his history, they realized his creatinine had been stable for months. His level was elevated-but not because his heart was failing. It was his kidneys. He didn’t need a new drug. Just better fluid management. These aren’t edge cases. They’re everyday moments where the right test changes the trajectory.What’s the difference between NT-proBNP and BNP?
NT-proBNP is the inactive fragment of the same hormone as BNP, but it’s more stable in the blood. BNP breaks down quickly-its half-life is about 20 minutes-so it’s harder to measure accurately if samples are delayed. NT-proBNP lasts 60-120 minutes, making it more reliable in real-world settings. NT-proBNP also has slightly higher diagnostic accuracy, with better correlation to heart function on echocardiograms. Most labs now prefer NT-proBNP for these reasons.
Can NT-proBNP be used to monitor heart failure treatment?
It can, but not routinely. A single baseline test is most valuable for diagnosis. Repeated testing is useful if you’re adjusting therapy in a patient with worsening symptoms or after hospital discharge. Falling levels often mean treatment is working. Rising levels may signal decompensation. But you shouldn’t order it weekly or monthly just because someone has heart failure-focus on symptoms and clinical signs instead.
Is NT-proBNP testing covered by insurance in Australia?
Yes, under Medicare in Australia, NT-proBNP testing is covered when ordered for suspected heart failure or acute dyspnea. It’s classified as a diagnostic test under the Medical Benefits Schedule (MBS). However, if ordered for asymptomatic patients or without clear clinical indication, it may be denied. Always ensure the reason for testing is documented in the patient’s record.
What if NT-proBNP is high but the patient feels fine?
That’s called asymptomatic elevation. It happens in older adults, people with kidney disease, or those with long-standing high blood pressure. It doesn’t always mean heart failure is present, but it does mean the heart is under some strain. These patients should be monitored closely-watch for new symptoms like swelling, fatigue, or shortness of breath. A follow-up echo and review of medications (like NSAIDs or calcium channel blockers) is often recommended. Don’t ignore it, but don’t over-treat it either.
Can obesity or kidney disease make NT-proBNP results unreliable?
Yes, but not in the way most people think. Obesity lowers NT-proBNP levels, so a normal result in a very overweight person doesn’t rule out heart failure-you need to look at symptoms harder. Kidney disease raises NT-proBNP levels because the kidneys can’t clear it well. That means the cutoff values need to be adjusted upward in patients with moderate to severe CKD. Use the modified ESC cutoff of <1,200 pg/mL for rule-out in stage 3-5 CKD, especially in older adults. Always interpret the number in context.