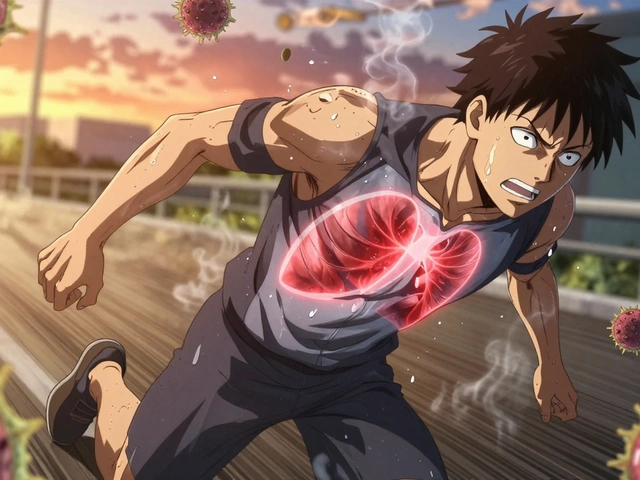
When you take one sedating medication, it might make you sleepy. Take two, and suddenly you’re struggling to stay awake-even if you didn’t plan to. This isn’t just about feeling tired. It’s about your breathing slowing down, your brain shutting off, and your body losing control. Every year, thousands of people end up in emergency rooms or worse because they didn’t realize how dangerous combining sedating drugs can be. And it’s not just opioids and sleeping pills. Alcohol, antidepressants, muscle relaxants, even some over-the-counter cold medicines can turn a harmless routine into a life-threatening mix.
What Happens When Sedating Drugs Combine?
Most sedating medications work the same way: they boost the effect of a brain chemical called GABA. This slows down your nervous system, which is why they help with anxiety, insomnia, or seizures. But when you take two or more of these drugs at once, they don’t just add up-they multiply. That’s called synergy. One pill might make you drowsy. Two together can stop your breathing.
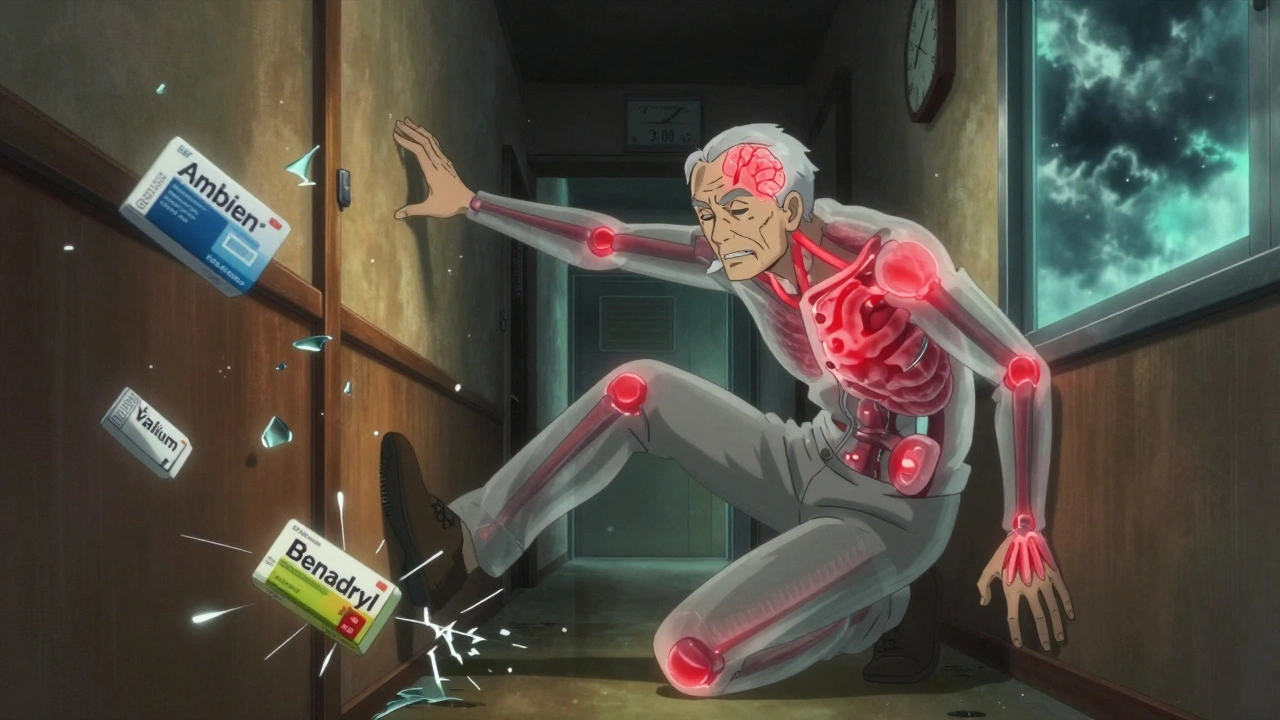
The most dangerous combination is opioids and benzodiazepines. Opioids like oxycodone or hydrocodone calm pain by targeting brain receptors. Benzodiazepines like Xanax or Valium calm nerves by boosting GABA. Together, they hit the brainstem-the part that controls breathing-and shut it down. A 2017 study in JAMA Internal Medicine found people taking both had more than double the risk of overdose compared to those taking opioids alone. The risk jumps even higher if alcohol is added. Just two drinks with a sleep aid like Ambien can cut reaction time by 70%, making falls, car crashes, and accidents far more likely.
Warning Signs You’re in Danger
These aren’t vague symptoms. These are red flags that mean your body is failing. If you or someone you know is taking multiple sedatives and shows any of these, call emergency services immediately:
- Slowed breathing-fewer than 12 breaths per minute
- Blue lips or fingertips-sign of low oxygen
- Unresponsiveness-can’t wake up even with loud shouting or shaking
- Gurgling sounds when breathing-like water in the throat
- Extreme confusion or slurred speech that’s worse than usual
Many people dismiss these signs as ‘just being tired’ or ‘having a bad night.’ But when multiple sedatives are involved, there’s no safe level of drowsiness. That groggy feeling? It’s your body screaming for help.
Who’s Most at Risk?
Older adults are especially vulnerable. As we age, our bodies process drugs slower. Liver and kidney function decline. Even low doses can build up. The American Geriatrics Society’s Beers Criteria lists 19 dangerous sedating combinations to avoid in people over 65. One of the biggest risks? Falls. Sedatives mess with balance and judgment. One in three older adults who take multiple sedating drugs will fall in a year-and many of those falls lead to broken hips or brain injuries.
People with chronic pain, anxiety, or insomnia are also at high risk. It’s common for someone with chronic pain to get an opioid, then a benzodiazepine for sleep, then an antidepressant for mood. Each prescription makes sense on its own. Together? A perfect storm. A 2020 study found that only 17% of electronic health record systems flagged these dangerous combinations, meaning doctors often don’t even know what their patients are taking.
Common Dangerous Combinations (And What to Do)
Here are the most frequent-and deadly-mixes:
- Opioids + Benzodiazepines: Highest risk of fatal overdose. The FDA issued a boxed warning in 2022 requiring all prescriptions to include this risk.
- Alcohol + Any Sedative: No safe amount. Even one drink with Ambien or Valium can be deadly. Alcohol doesn’t just add to the effect-it makes it unpredictable.
- SSRIs + MAOIs: This mix can trigger serotonin syndrome, a life-threatening condition where your body overheats, your heart races, and your muscles lock up. A 14-day washout period is required when switching between these antidepressants.
- Benzodiazepines + Muscle Relaxants: Both depress the central nervous system. Combining them increases dizziness, confusion, and risk of falls.
- OTC Sleep Aids + Prescription Sedatives: Many people don’t realize diphenhydramine (Benadryl, ZzzQuil) is a sedative. Taking it with a sleep prescription is like doubling the dose.
There’s no such thing as a ‘safe’ combo unless it’s carefully monitored by a doctor who knows every drug you’re taking-including vitamins, herbs, and supplements. Melatonin, kava, valerian root-all can add to sedation.
What You Can Do Right Now
You don’t need to wait for your next appointment. Start today:
- Make a full list of everything you take: prescriptions, over-the-counter meds, supplements, even herbal teas. Include doses and how often you take them.
- Bring that list to your doctor or pharmacist. Ask: ‘Could any of these interact dangerously?’ Don’t assume they know what you’re taking-many don’t.
- If you’re on opioids and a benzodiazepine, ask if there’s a non-sedating alternative for anxiety or sleep. Cognitive behavioral therapy for insomnia (CBT-I) works better than pills for most people.
- Never drink alcohol while on sedatives. Not even one glass.
- Teach someone close to you the warning signs. If you can’t speak for yourself, they need to know when to call 911.
Some people think, ‘I’ve been taking these for years without problems.’ That’s not proof it’s safe-it’s luck. The body changes. Tolerance builds. A dose that was fine last year might be dangerous now.

Why Doctors Still Prescribe Dangerous Combos
It’s not that doctors are careless. Many are trapped by the system. Pain patients get opioids because there aren’t enough non-addictive alternatives. Anxiety sufferers get benzodiazepines because therapy is expensive and hard to access. Sleep aids are quick fixes when CBT-I isn’t covered by insurance. And many doctors don’t have time to review all 10+ medications a patient might be taking.
But change is happening. The SUPPORT Act of 2018 forced Medicare Part D plans to screen for opioid-benzodiazepine combos. The FDA now requires stronger warnings. AI tools like DETERMINE can now predict individual risk with 87% accuracy. But these systems are still new. Most primary care providers still don’t routinely screen for dangerous combinations.
Your safety can’t depend on a computer alert. It depends on you asking questions, speaking up, and refusing to accept ‘it’s fine’ when something feels off.
When to Seek Help
If you’re taking multiple sedatives and you feel:
- More confused than usual
- Like you’re walking through fog
- Unable to get out of bed without help
- Like your breathing is shallow or irregular
-it’s not normal. It’s not just aging. It’s a medical emergency waiting to happen.
Don’t wait for a crash. Talk to your doctor about tapering off one drug at a time. Never quit cold turkey-especially benzodiazepines. Withdrawal can cause seizures. But with proper medical supervision, most people can safely reduce their doses and find better, non-sedating solutions.
The goal isn’t to live on pills. It’s to live without them.
Can I just cut my dose in half to avoid the risks?
No. Reducing your dose without medical guidance can be dangerous, especially with benzodiazepines or opioids. Withdrawal can cause seizures, severe anxiety, or rebound insomnia. Always work with your doctor to create a safe tapering plan-usually reducing by 10-25% every 1-2 weeks.
Are natural sleep aids like melatonin safe with sedatives?
Not necessarily. Melatonin, valerian root, kava, and even chamomile tea can enhance sedation. While they’re not as strong as prescription drugs, they still add up. If you’re taking a sleeping pill, avoid herbal sleep aids unless your doctor says it’s safe.
What should I do if I suspect someone is overdosing on sedatives?
Call emergency services immediately. If you have naloxone (Narcan) and the person is on an opioid, administer it. But naloxone won’t reverse benzodiazepine or alcohol overdose. Keep the person awake and on their side until help arrives. Don’t give them coffee or let them ‘sleep it off’-that can be fatal.
Can I take a sedative for a bad night and then another the next day?
No. Even spacing them out doesn’t eliminate risk. Many sedatives build up in your system over days. Taking one daily-even at low doses-can lead to accumulation. This is especially true for older adults. Talk to your doctor about long-term alternatives like CBT-I instead of relying on nightly pills.
Why don’t pharmacists warn me about these combinations?
They should-but many don’t have full access to your complete medication list. If you fill prescriptions at multiple pharmacies or use online services, your records may be split. Always bring your full list to the pharmacy. Ask: ‘Is this safe with everything else I take?’ Don’t assume they know.
Are there non-sedating alternatives for anxiety or insomnia?
Yes. For anxiety, SSRIs like sertraline or escitalopram are first-line and don’t cause sedation long-term. For insomnia, CBT-I is more effective than any pill and has lasting results. Other options include light therapy, mindfulness, and regular exercise-all proven to improve sleep without drugs. Ask your doctor about referrals.
Final Thought: Your Life Is Worth More Than a Quick Fix
There’s no shame in needing help with sleep, pain, or anxiety. But using multiple sedatives to manage them is like driving with the brakes and gas pressed at the same time. You might think you’re in control-but you’re not. The system is stacked against you. Pills are cheap. Therapy isn’t. Warnings are buried in fine print. Doctors are rushed. But you have power: you can ask questions. You can say no. You can demand better.
One less pill. One fewer interaction. One more day awake and clear-headed. That’s the goal. Not more drugs. More life.





Lisa Whitesel
December 10, 2025 AT 14:54Stop pretending this is news. People die every day from mixing meds and no one cares until it's their kid.
Doctors prescribe like they're playing Jenga. You pull one out, everything collapses.
It's not complicated. Stop being lazy. Ask questions. Or die. Your call.
Ryan Brady
December 10, 2025 AT 21:00USA needs to stop coddling weak people who can't handle a little sleep aid and a pain pill.
My grandpa took 3 different sedatives for 40 years and still mowed his lawn at 82.
Liberal medicine is killing us. 🇺🇸💀
Darcie Streeter-Oxland
December 11, 2025 AT 16:59It is, without question, a matter of profound public health concern that the concomitant administration of multiple central nervous system depressants remains so prevalent within clinical practice.
The synergistic potentiation of GABAergic activity, coupled with the insidious nature of cumulative pharmacokinetic effects, renders this phenomenon not merely hazardous but, in many instances, lethally predictable.
Regrettably, systemic failures in pharmacovigilance and patient education continue to perpetuate this crisis.
Taya Rtichsheva
December 12, 2025 AT 00:21so like... benzos + opioids + alcohol + melatonin + chamomile tea = death soup?
lol. i guess i'm just lucky i haven't died yet.
also my doctor never asked about my kava tincture. oops.
weird how no one ever talks about the herbal stuff til you're already half-dead 😅
Mona Schmidt
December 13, 2025 AT 13:29This is one of the most important public health messages I've seen in years.
Many people don't realize that even "natural" supplements like valerian or kava can interact dangerously with prescription sedatives.
It's not about fear-mongering-it's about informed consent.
Every patient deserves to know the full scope of risk, not just the benefit.
Pharmacists should be required to review all medications, including OTC and supplements, during every dispensing.
And doctors need better tools to see the whole picture-not just the last 3 prescriptions.
CBT-I is underutilized because insurance won't pay for it, not because it doesn't work.
We need policy change, not just awareness.
Thank you for writing this with such clarity.
People are dying because we treat symptoms instead of root causes.
Let’s stop normalizing polypharmacy as "just part of aging."
It’s not normal. It’s a failure of care.
And if you’re on more than two sedatives, you deserve a thorough review-not just a refill.
Guylaine Lapointe
December 14, 2025 AT 14:01People who say "I've been taking these for years" are just lucky, not smart.
And don't tell me about your uncle who "took Xanax and whiskey every night and lived to 90"-that's an outlier, not a lifestyle.
My mom died from a "quiet overdose"-no struggle, no noise, just stopped breathing one night.
They called it "natural causes."
It wasn't.
She was on 5 meds that should never have been together.
And the doctor didn't know half of them because she filled them at 3 different pharmacies.
Stop pretending this is rare.
It's happening in every suburb, every nursing home, every family who thinks "it's fine."
It's not fine.
And if you're reading this and you're on more than two sedatives? Please, for God's sake, make a list. Talk to someone. Don't wait for the gurgling.
Sarah Gray
December 15, 2025 AT 21:33Oh look, another sanctimonious pamphlet from the pharmaceutical fear-mongering industrial complex.
People have been mixing meds since the 1950s.
Where were you when my grandfather took Librium and bourbon for 30 years and never had a problem?
It’s not the drugs-it’s the weak minds who can’t handle responsibility.
And why do you assume everyone is a helpless elder? I’m 32 and on three sedatives-because I have chronic pain, anxiety, and insomnia.
My doctor is brilliant. My pharmacist is attentive.
Stop treating adults like children who need a lecture.
You’re not saving lives-you’re infantilizing them.
Kathy Haverly
December 15, 2025 AT 23:42Oh wow. Another "wake up sheeple" post from someone who clearly doesn’t understand addiction.
You think people are taking these because they’re dumb?
No. They’re taking them because the system failed them.
Therapy costs $200/hour.
CBT-I has a 2-year waitlist.
Doctors get paid to prescribe, not to listen.
And you think a list of meds is going to fix that?
Pathetic.
Meanwhile, Big Pharma is laughing all the way to the bank while you preach to the choir.
Stop pretending you’re helping.
You’re just making people feel guilty for surviving.
Andrea Petrov
December 16, 2025 AT 08:30Did you know the FDA’s warning labels are designed to make you feel safe so you keep taking the pills?
It’s all a setup.
They want you dependent.
They know combining sedatives kills-but they keep approving them anyway.
And your "doctor"? They’re on payroll from the same companies that make the drugs.
They don’t want you off them.
They need you to keep buying.
That’s why they don’t mention melatonin or kava-they’re not profitable.
And don’t even get me started on how your pharmacy records are being sold to data brokers.
You think this is about safety?
No.
It’s about control.
And they’re using your fear to keep you docile.
Suzanne Johnston
December 17, 2025 AT 10:16There is a quiet tragedy here that transcends pharmacology.
It is not merely the chemical synergy that kills-it is the erosion of human connection.
When we treat pain with pills instead of presence, when we manage insomnia with chemicals rather than community, we lose something irreplaceable.
Perhaps the real danger is not the combination of drugs, but the isolation that drives us to them.
We have built a society where suffering is commodified, not comforted.
And in that silence, the drugs become our only companions.
Let us not only warn of the chemistry-but restore the humanity.
George Taylor
December 18, 2025 AT 02:50Okay, but... have you considered that maybe the problem isn't the drugs... it's the fact that we're all just... so tired?
Like, seriously.
Work 60 hours a week.
Pay $3k/month in rent.
Try to sleep with a kid screaming in the next room.
Then go to the doctor and say, "I can't function."
And they hand you a script.
And you take it.
And then you take another.
And then you drink.
Because what else are you supposed to do?
It's not that people are stupid.
It's that the world is broken.
And now you're mad at us for trying to survive?
That's rich.
Also, I took 4 different sedatives last week. I'm fine.
Maybe I'm just built different.
Or maybe you just don't get it.
Peace.
ian septian
December 18, 2025 AT 18:59Make a list.
Ask your doctor.
Don’t drink.
Teach someone the signs.
Do it today.
Chris Marel
December 19, 2025 AT 16:34I come from a place where access to doctors is rare, and medicine is often shared among family.
My cousin took his father’s pain pills with his mother’s sleep aid because they both said they "felt better."
He didn’t wake up.
That was three years ago.
I still see his mother every Sunday.
She never talks about it.
But I see her holding his pill bottle like a prayer.
This isn’t just a warning.
It’s a memory.
Please, for the love of everyone you know-ask before you take.