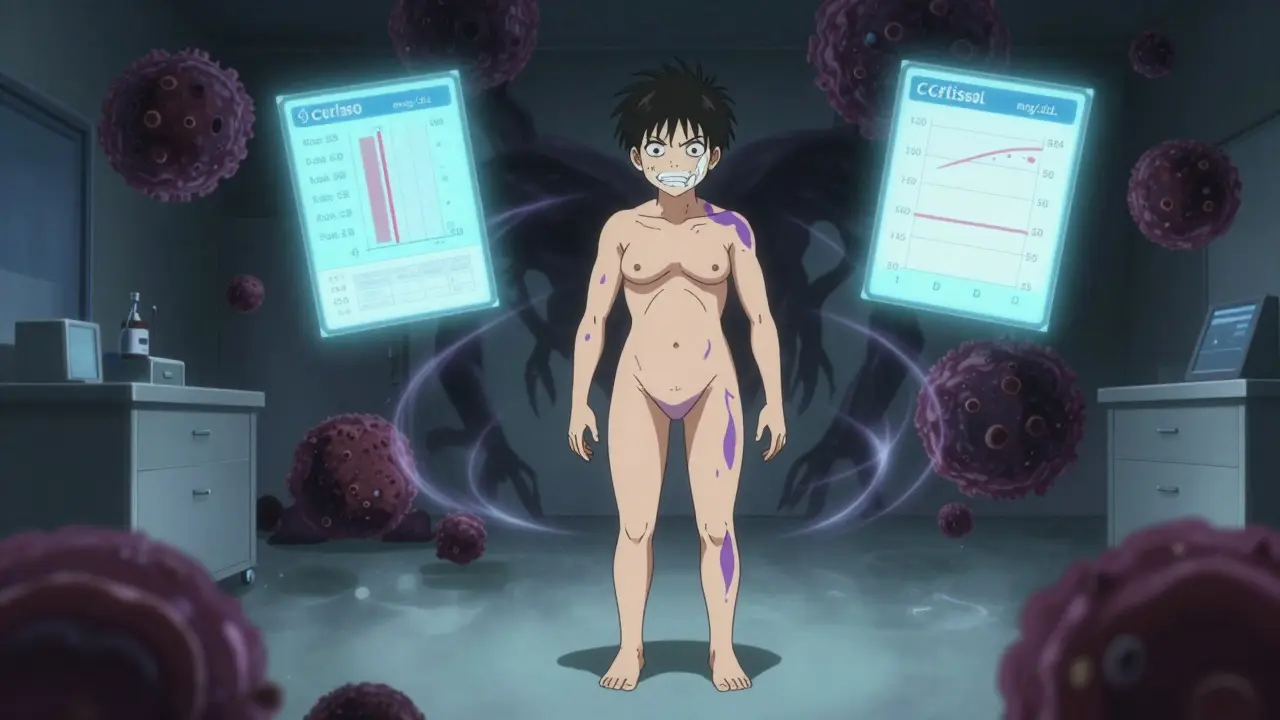
When your body makes too much cortisol - the stress hormone that keeps you alert, regulates blood sugar, and controls inflammation - it doesn’t just make you feel on edge. It rewires your body. Your face swells into a round, moon-like shape. Fat piles onto your abdomen while your arms and legs stay thin. Purple stretch marks appear on your skin like bruises that won’t fade. Your bones weaken. Your blood pressure spikes. You get tired all the time, even after a full night’s sleep. This isn’t just being stressed out. This is Cushing’s syndrome.
What Exactly Is Cushing’s Syndrome?
Cushing’s syndrome happens when your body is flooded with cortisol for too long. Normal cortisol levels range between 5 and 25 mcg/dL over 24 hours. In Cushing’s, they often climb above 50 mcg/dL - sometimes much higher. That’s like running your engine at redline for months on end. Eventually, something breaks. There are two main types. The first, and most common, is exogenous Cushing’s - caused by taking steroid medications like prednisone for conditions like asthma, lupus, or rheumatoid arthritis. About 80% of cases fall into this category. The second, and more complex, is endogenous Cushing’s - where your own body overproduces cortisol. This happens in about 20% of cases, and it’s the kind that usually needs surgery. Endogenous Cushing’s is typically caused by a tumor. Most often, it’s a tiny, noncancerous growth in the pituitary gland (called a pituitary adenoma) that sends out too much ACTH, the hormone that tells your adrenal glands to make more cortisol. This version is called Cushing’s disease, and it accounts for 60-70% of all endogenous cases. Less common causes include tumors on the adrenal glands themselves (15-20%) or tumors elsewhere in the body - like the lungs or pancreas - that accidentally start producing ACTH (5-10%).How Do You Know If You Have It?
Cushing’s doesn’t show up on a regular blood test. It sneaks in slowly. Many people think they’re just gaining weight, or their skin is getting thin, or they’re getting more irritable. It takes time - often years - before someone connects the dots. Doctors look for a cluster of signs:- Moon face - a round, flushed face with full cheeks
- Buffalo hump - a fatty lump between the shoulders
- Central obesity - belly fat that grows fast while arms and legs stay skinny
- Violaceous striae - wide, purple stretch marks on the abdomen, thighs, or breasts
- Easy bruising and thin skin
- High blood pressure (in 85% of patients)
- High blood sugar or diabetes (70% of cases)
- Osteoporosis - bones so weak they break easily (T-score below -2.5 in half of patients)
- 24-hour urine cortisol test - if you’re excreting more than 50 mcg in a day, that’s a red flag
- Low-dose dexamethasone suppression test - if your cortisol doesn’t drop after taking a steroid pill, your body isn’t regulating itself properly
- Late-night salivary cortisol - cortisol should be near zero at night. If it’s above 0.14 mcg/dL, something’s wrong
Why Surgery Is the First-Line Treatment
If you have endogenous Cushing’s and a tumor is the cause, surgery isn’t just an option - it’s the best shot at a cure. Medications like pasireotide or mifepristone can help manage symptoms, but they don’t remove the source. They’re like putting a bandage on a broken pipe. Surgery fixes the leak. The Endocrine Society’s 2020 guidelines are clear: for pituitary or adrenal tumors, surgery should come before any drug treatment. Why? Because the success rates are far higher. For pituitary tumors (Cushing’s disease), the go-to surgery is transsphenoidal surgery. The surgeon goes through the nose or upper lip, into the sphenoid sinus, and removes the tumor without cutting into the brain. It takes 2-4 hours. Most people are out of the hospital in 2-5 days. Success depends on two things: tumor size and surgeon experience. For small tumors under 10 mm, remission rates are 80-90%. For larger ones, it drops to 50-60%. And here’s the kicker: centers that do fewer than 10 of these surgeries a year have remission rates as low as 50-60%. High-volume centers - those doing 20 or more per year - hit 80-90%. That’s the difference between hope and certainty.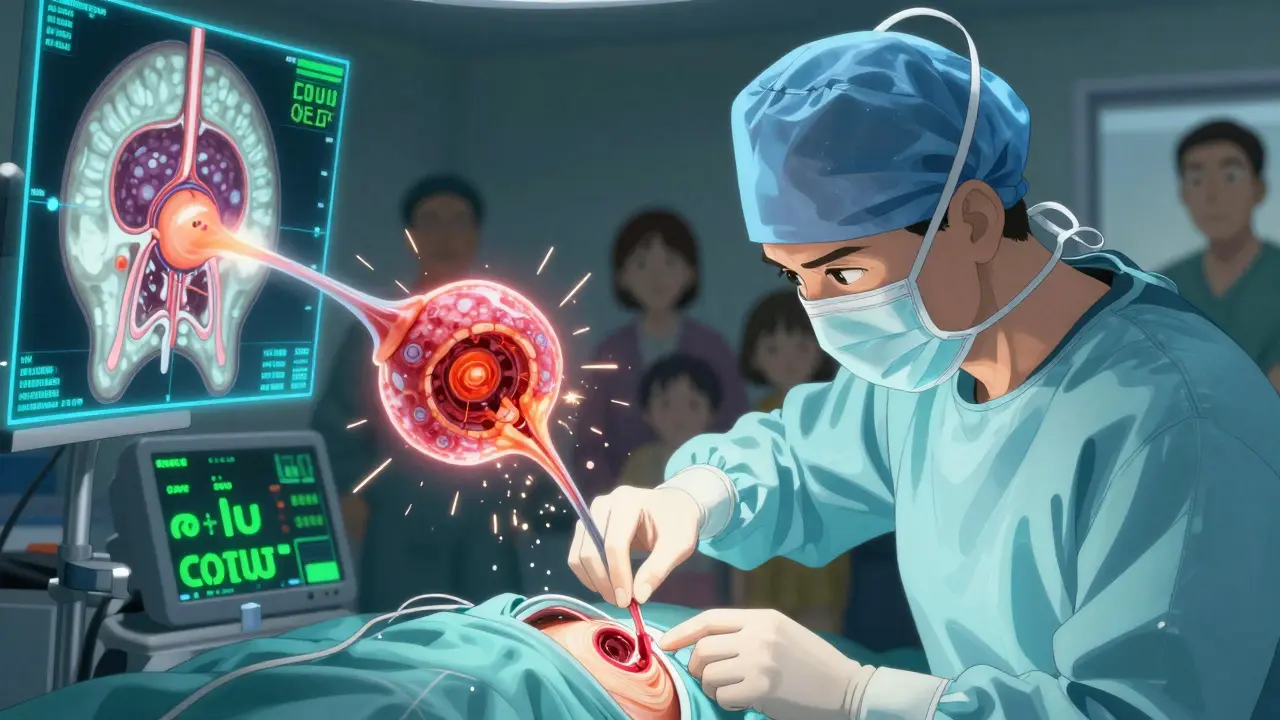
Adrenal Surgery: When the Problem Is on the Glands
If the tumor is on one adrenal gland, the fix is simpler: a laparoscopic adrenalectomy. The surgeon makes three small cuts in the abdomen, inserts a camera and tools, and removes the gland. It takes 1-2 hours. Hospital stay? Usually just 1-2 days. Success rate? Around 95%. Most people go home with cortisol levels back to normal. Complications are rare - bleeding or infection happens in just 2-5% of cases. But if both adrenal glands are overactive - say, from a rare condition called bilateral macronodular hyperplasia - removing both might be necessary. This is called bilateral adrenalectomy. It cures the cortisol problem completely. But now, your body can’t make cortisol at all. Ever again. That means lifelong steroid replacement. You’ll need hydrocortisone and fludrocortisone every day. And there’s a serious risk: Nelson’s syndrome. In up to 40% of cases, the pituitary tumor grows back aggressively, causing darkening of the skin, headaches, and vision problems. That’s why this surgery is only done when other options have failed.The Real Cost of Surgery - Beyond the Operating Room
Surgery doesn’t end when you wake up. The real challenge starts after. Your body has been flooded with cortisol for so long that it stopped making its own. After the tumor is removed, your adrenal glands are basically asleep. For weeks or months, you’ll need to take replacement steroids - often in doses higher than your body ever needed before. Then, slowly, you taper down. About 30-40% of patients have temporary adrenal insufficiency. For 5-10%, it’s permanent. You’ll need to learn how to adjust your dose during illness, injury, or stress. If you get the flu and don’t increase your steroids, you could go into adrenal crisis - low blood pressure, vomiting, fainting. It can be deadly. Recovery takes time. Most people report feeling better in 3-6 months. But full recovery - energy levels, muscle strength, mood - can take up to a year. One patient, Jane_D, wrote on a support forum: “Two months after surgery, my moon face vanished. My blood pressure went normal without meds. I lost 40 pounds.” But another, Mark_T, said: “I still have chronic fatigue. I need thyroid and testosterone replacements now.” And it’s not just physical. Many people struggle with body image. The weight gain, the skin changes - they don’t vanish overnight. Therapy and support groups help. The Cushing’s Support & Research Foundation reports that 85% of patients feel significantly better by 12 months post-op. But 15% still need more treatment.





rachel bellet
January 17, 2026 AT 23:47Let’s be clear: this isn’t ‘stress’-it’s a systemic endocrine catastrophe. The diagnostic delay is unconscionable. The 24-hour urinary free cortisol test remains gold standard, yet primary care providers still rely on ‘clinical suspicion’ instead of protocol-driven screening. And don’t get me started on the dexamethasone suppression test misinterpretations-seriously, if your cortisol doesn’t suppress below 1.8 mcg/dL after 1 mg overnight, you’re not ‘just tired.’ You’re in Cushing’s. Period. The literature is unequivocal: failure to act within 12 months of symptom onset correlates with irreversible metabolic and neuropsychiatric damage. This isn’t opinion. It’s evidence-based medicine.
Jay Clarke
January 19, 2026 AT 00:34Bro. I had a cousin go through this. She looked like a cartoon villain by the time they figured it out. Moon face? Check. Purple stretch marks? Like she got in a fight with a zipper. And the worst part? She was told for YEARS she was ‘just eating too much.’ Like, what? You think cortisol makes you crave pizza? Nah. It’s your body turning into a stress-powered meat puppet. Surgery fixed her. But now she’s on meds for life. And she cries in the shower sometimes. This isn’t just a ‘hormone thing.’ It’s a whole life reset. And nobody talks about that.
Selina Warren
January 20, 2026 AT 00:06Listen. I know what it’s like to feel like your body is betraying you. I’ve been there. But here’s the truth: surgery isn’t the end-it’s the beginning of your rebirth. You think the weight’s gonna vanish overnight? Nope. But the fog? The exhaustion? The crushing dread? That lifts. I remember the first morning I woke up and didn’t feel like I was drowning in molasses. That was day 47 post-op. I cried. Not from pain-from freedom. You’re not broken. You’re just waiting for your body to remember how to breathe. And guess what? You can. You will. And when you do, you’ll be stronger than you ever imagined. This isn’t a diagnosis. It’s a doorway. Walk through it.
Nishant Sonuley
January 21, 2026 AT 10:55Interesting piece, though I must say, the emphasis on surgical intervention overlooks the broader systemic failures in endocrine care. In India, where I’m from, access to high-volume pituitary centers is nearly nonexistent outside metro cities. Even if you can afford it, the waitlist is 18 months. And let’s be honest-why are we treating the symptom (the tumor) and not the root? What’s causing these tumors? Environmental toxins? Chronic stress? Genetic predisposition? The article reads like a surgical manual, but where’s the public health lens? We need screening programs, not just high-tech fixes for the privileged few. Also, ‘lifelong steroid replacement’ is a euphemism for ‘you’re now a medical dependent.’ That’s not cure. That’s management. And management isn’t justice.
Emma #########
January 22, 2026 AT 05:38I just wanted to say thank you for writing this. I was diagnosed last year. I didn’t even know what Cushing’s was until my endocrinologist said it. I thought I was just depressed and lazy. Reading this made me feel seen. The part about body image… yeah. I still avoid mirrors sometimes. But I’m getting there. One day at a time.
Andrew McLarren
January 23, 2026 AT 01:25While the clinical accuracy of this exposition is commendable, one must acknowledge the ethical imperative to contextualize surgical intervention within the broader framework of patient autonomy and informed consent. The assertion that surgery is ‘the best shot at a cure’ may inadvertently marginalize those for whom surgical risk outweighs benefit-particularly those with comorbidities or advanced age. A multidisciplinary approach, inclusive of pharmacological, behavioral, and palliative modalities, must be presented not as a secondary option, but as a legitimate and dignified pathway. The goal is not merely remission, but quality of life as defined by the patient, not the protocol.
Andrew Short
January 23, 2026 AT 06:22Let’s cut through the fluff. This is Big Pharma’s masterpiece. Steroids? Easy to patent. Lifelong meds? Infinite revenue stream. Surgery? One-time payment. So they make you wait years for diagnosis, then sell you drugs while they wait for you to get desperate enough to cut yourself open. And guess what? The ‘success rates’? They’re inflated. Surgeons call it ‘remission’ when cortisol drops-ignoring the fact that your adrenal glands are dead. You’re not cured. You’re chemically maintained. And the real winners? The hospitals charging $100K for a 3-hour nose job. Wake up. This system doesn’t want you healed. It wants you dependent.
christian Espinola
January 23, 2026 AT 06:47Correction: ‘Cushing’s disease’ refers ONLY to pituitary adenoma-driven hypercortisolism. The term ‘Cushing’s syndrome’ encompasses ALL causes-including exogenous steroid use. The article conflates them repeatedly. Also: ‘late-night salivary cortisol above 0.14 mcg/dL’-incorrect. The cutoff is 0.10 mcg/dL per 2023 Endocrine Society guidelines. And ‘11C-metomidate PET/CT’ is not ‘in trials’-it’s FDA-cleared and available at select centers since 2022. These aren’t typos. They’re dangerous inaccuracies. If you’re going to publish medical content, at least read the latest guidelines. Otherwise, you’re contributing to diagnostic delay.
Chuck Dickson
January 23, 2026 AT 07:01Hey-just wanted to say you’re not alone. I had the surgery last year. Lost 50 lbs. Got my energy back. Still take steroids, but I can run now. I used to cry every night. Now I coach a kids’ soccer team. You think this is the end? Nah. This is the beginning of the life you were supposed to have. I know it feels like the world’s against you. But you’ve already won just by reading this. You’re looking for answers. That’s courage. And courage gets you through the dark. I’m rooting for you.
Robert Cassidy
January 23, 2026 AT 10:03They don’t want you to know this, but Cushing’s is a weaponized disease. The government knows cortisol manipulation can break people. That’s why they let it go undiagnosed for years-keeps the population docile. Fat, tired, confused. Perfect for control. And now they sell you a ‘cure’ that leaves you dependent on pills. That’s not medicine. That’s psychological warfare. They don’t care if you live-they care if you obey. And the ‘specialized centers’? They’re just fronts for the same system. Wake up. This isn’t biology. It’s control.
Naomi Keyes
January 24, 2026 AT 21:41