Living with diabetic neuropathy pain isn’t just about discomfort-it’s about losing control. Your feet, once reliable and strong, now burn, tingle, or feel numb without warning. Simple things like walking to the mailbox or putting on socks become challenges. And no matter how hard you try to manage your blood sugar, the nerve damage doesn’t reverse. That’s the hard truth: diabetic neuropathy pain can’t be cured yet. But it can be managed. And managing it well means two things: the right medications and disciplined foot care.
What Medications Actually Work for Diabetic Neuropathy Pain?
The FDA has approved only four drugs specifically for diabetic neuropathy pain: duloxetine, pregabalin, tapentadol extended-release, and the 8% capsaicin patch. But doctors often use others off-label because not everyone responds the same way. The goal isn’t to make pain disappear completely-it’s to reduce it by 30% to 50%. That’s the average improvement seen in clinical trials, and for many, that’s enough to get through the day.
Duloxetine (Cymbalta) is often the first choice. It’s an SNRI, meaning it helps with both pain and depression-something many people with chronic nerve pain also struggle with. Studies show it reduces pain by about half in responsive patients. It takes about three weeks to reach full effect, and the standard dose is 60 mg once daily. One big plus? Generic duloxetine costs around $15 for a 90-day supply. That’s a huge difference compared to brand-name options.
Pregabalin (Lyrica) is another top option. It works fast-some people feel relief within 48 hours. But it comes with trade-offs. About 30% of users get dizzy, and 20% feel overly sleepy. It’s also expensive, even as a generic: $378 for 90 capsules. Still, it’s one of the most studied drugs for this condition, with over 16 high-quality trials backing its use. It also helps with sleep and anxiety, which often get worse with chronic pain.
Gabapentin is cheaper-just $4 for 90 capsules-and widely used, even though it’s not FDA-approved for diabetic neuropathy. It’s often prescribed at doses between 900 mg and 3,600 mg daily, split into three doses. But it’s not as effective as duloxetine or pregabalin in head-to-head studies. Many people stop taking it because the dizziness and brain fog are too much.
Tricyclic antidepressants like amitriptyline are still recommended by experts, even though they’re not FDA-approved for this use. They work well for some, especially at low doses (10-50 mg at bedtime). But side effects are common: dry mouth, constipation, blurred vision, and weight gain. People over 45 need heart monitoring because these drugs can affect heart rhythm.
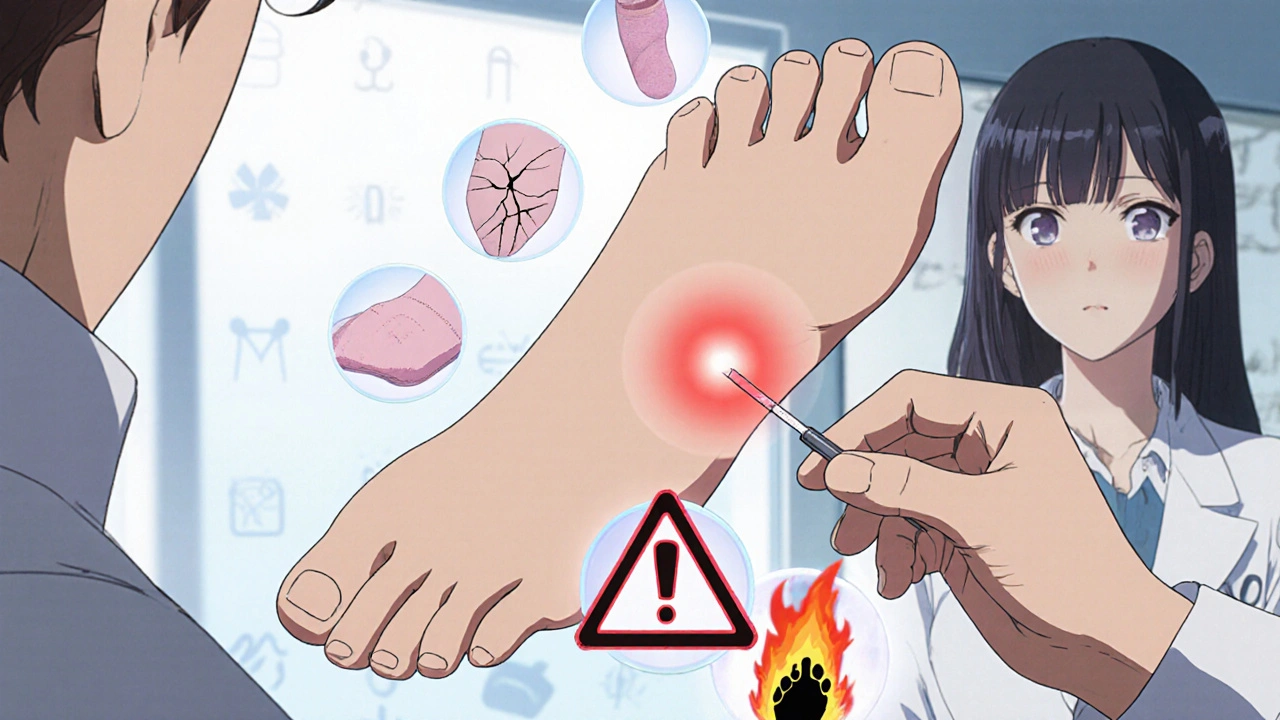
The 8% capsaicin patch (Qutenza) is a game-changer for foot pain. Applied by a healthcare provider, it numbs the nerves in your feet for up to three months. One patient on Reddit said it cut his pain by 70%. But the application? Painful. You feel a burning sensation during the 30-minute procedure. Not for everyone, but for those with localized foot pain, it’s worth considering.
What Doesn’t Work-or Can Hurt You
Many people reach for over-the-counter painkillers like ibuprofen or naproxen. Don’t. NSAIDs can damage your kidneys, and people with diabetes already have a 2.1 times higher risk of acute kidney injury from these drugs. Even at normal doses, it’s dangerous.
Opioids like tramadol or oxycodone are sometimes used, but they’re not a long-term solution. The CDC strongly advises against them for chronic nerve pain because of addiction risk. Studies show 3-12% of people on long-term opioids develop dependence. Tramadol is only recommended as a third-line option by the NHS, after everything else fails. And even then, it’s used with caution.
There’s no magic pill. Every medication has side effects. The key is starting low, going slow, and giving each drug at least 4 to 8 weeks to work. If one doesn’t help after that, your doctor will switch you to another. It’s trial and error-but it’s not random. It’s based on evidence, your other health issues, and what you can tolerate.
Foot Care Isn’t Optional-It’s Life-Saving
Medications help with pain, but foot care stops the worst outcomes: ulcers, infections, and amputations. One in five people with diabetic neuropathy will develop a foot ulcer within five years. And once an ulcer forms, the risk of losing a toe or foot jumps dramatically.
Here’s what you need to do every single day:
- Check your feet for cuts, blisters, redness, swelling, or sores. Use a mirror if you can’t see the bottom of your feet.
- Wash your feet daily in lukewarm water. Test the temperature with your elbow-your feet can’t feel if it’s too hot.
- Dry them thoroughly, especially between the toes. Moisture breeds fungus and infection.
- Apply moisturizer to keep skin soft, but never between the toes.
- Never go barefoot-not even inside. Wear shoes or slippers at all times.
- Trim your toenails straight across. Don’t cut into the corners.
- Wear socks made for diabetics: no seams, no tight bands, moisture-wicking fabric.
Annual foot exams by your doctor are non-negotiable. They use a 10-gram monofilament to test sensation in your feet. If you can’t feel the light touch, you’re at high risk. That’s when you need custom footwear or orthotics. Medicare and most insurance plans cover these if you have neuropathy.
Real People, Real Results
One 62-year-old man in Australia tried gabapentin, amitriptyline, and pregabalin before switching to duloxetine. His pain dropped 65%. He also noticed his mood improved-he hadn’t realized how much the pain had been dragging him down.
A woman in Melbourne stopped using oral meds after trying the capsaicin patch. She still checks her feet every morning and wears diabetic socks. She says, “The patch didn’t fix everything, but it gave me back my mornings.”
But not everyone succeeds. One man on a diabetes forum said he quit amitriptyline because the dry mouth and constipation were worse than the pain. He ended up with a foot ulcer because he stopped checking his feet regularly. “I thought if the pain was gone, I was fine,” he admitted. “I was wrong.”
What’s Coming Next
Research is moving fast. A new drug called mirogabalin just got FDA approval in late 2023 and may offer better pain relief with fewer side effects. Studies are also looking at combining pregabalin with N-acetylcysteine-early results show pain reduction up to 100% in some patients.
There’s also emerging science on genetic testing. A 2023 study found that people with certain gene variations respond much better to duloxetine. In the future, your doctor might test your DNA before prescribing.
But none of this changes the basics. Until then, the most effective tools are still the ones we’ve had for years: the right meds, used wisely, and daily foot care that’s as routine as brushing your teeth.

When to Call Your Doctor
Don’t wait for a crisis. Call your doctor if:
- Your pain gets worse suddenly or changes in quality (e.g., sharp stabbing instead of burning).
- You notice a sore, blister, or red spot on your foot that doesn’t heal in 2 days.
- You develop swelling, warmth, or pus in your foot.
- You can’t feel your feet at all anymore.
- You’re having side effects from your medication that interfere with daily life.
Early action saves feet. And feet save lives.
Can diabetic neuropathy pain be reversed?
No, current treatments cannot reverse nerve damage caused by diabetes. The goal of therapy is to slow progression and reduce pain by 30-50%. Managing blood sugar tightly can prevent further damage, but existing nerve injury remains permanent. Research into regenerative therapies is ongoing, but nothing has been proven yet.
What’s the cheapest medication for diabetic neuropathy pain?
Gabapentin is the most affordable option, averaging $4 for a 90-day supply as a generic. Amitriptyline is also low-cost, often under $10. However, affordability doesn’t always mean best choice. Gabapentin has more side effects like dizziness and brain fog, while amitriptyline can cause dry mouth and heart rhythm issues. Always discuss cost with your doctor-they may have samples or patient assistance programs.
Do I need special shoes if I have diabetic neuropathy?
Yes, if you have lost sensation in your feet or have foot deformities like bunions or hammertoes. Custom diabetic shoes reduce pressure points and prevent ulcers. Medicare and most private insurers cover them if you have a diagnosis of diabetic neuropathy and a prescription from your doctor. Look for shoes with deep toe boxes, cushioned soles, and no internal seams.
Can I use heating pads or hot water bottles on my feet?
No. If you have neuropathy, you can’t feel heat properly. A heating pad or hot water bottle can burn your skin without you realizing it. Even lukewarm baths can be risky-always test water temperature with your elbow or a thermometer. Burns in neuropathic feet heal slowly and can lead to serious infections.
How long does it take for neuropathy medications to work?
Most medications take 2 to 6 weeks to show noticeable effects. Duloxetine and pregabalin often start helping within 1-2 weeks, but full benefit takes up to 12 weeks. Don’t stop them too soon. If you don’t see improvement after 8 weeks at the right dose, talk to your doctor about switching. Patience and consistency matter more than speed.
Next Steps for Better Control
Start today. Write down your current medications and side effects. Get a mirror if you can’t see your feet. Buy a pair of diabetic socks. Schedule your annual foot exam. And if your pain isn’t under control, ask your doctor about duloxetine or the capsaicin patch. You don’t have to live with pain that keeps you from moving. With the right tools, you can take back your life-one step at a time.





Kaylee Crosby
November 26, 2025 AT 00:55Just wanted to say this post saved my life honestly. I was about to quit on gabapentin because of the brain fog but now I know to give it 8 weeks. My feet still tingle but I can walk to the porch without crying. You’re not alone.
Adesokan Ayodeji
November 26, 2025 AT 19:19Man this is so true. In Nigeria we don’t have access to most of these meds, but I’ve been using neem leaf tea and coconut oil on my feet daily. Not science-backed but it helps with the burning. And I check my feet every morning before I even drink water. My uncle lost his foot because he thought the numbness meant it was getting better. Don’t make that mistake. Your feet are your roots, man. Water them, don’t ignore them.
Karen Ryan
November 27, 2025 AT 06:20Capasaicin patch? 😱 I tried it last year. The burn during application felt like someone poured lava on my toes. But 3 months of near-zero pain? Worth it. Also, diabetic socks = life. I got mine from Dr. Scholl’s. They don’t have seams and actually stay up. 👍🧦
Terry Bell
November 28, 2025 AT 20:59I used to think pain was just part of aging until I realized it was my body screaming for help. Duloxetine didn’t fix everything but it gave me back the mornings. I can now make coffee without wincing. That’s not a cure but it’s a gift. And yeah, foot checks are boring but so is being in a wheelchair. Choose your battles.
Lawrence Zawahri
November 29, 2025 AT 00:22THE PHARMA INDUSTRY IS LYING TO YOU. DULOXETINE IS JUST ANTIDEPRESSANT SLIME TO KEEP YOU DEPRESSED AND PAYING. THEY DON’T WANT YOU WELL. THEY WANT YOU ON MEDS FOREVER. THE CAPSAICIN PATCH? IT’S A TRAP. THEY’RE USING IT TO MAKE YOU THINK YOU’RE GETTING HELP WHILE THEY SELL YOU MORE DRUGS. CHECK THE FDA’S 2021 WHISTLEBLOWER REPORT. THEY’RE HIDING THE TRUTH. YOUR FEET AREN’T THE PROBLEM - THE SYSTEM IS.
Benjamin Gundermann
November 30, 2025 AT 05:17Look I get it, meds are expensive and the system sucks but come on. You’re telling people to use gabapentin because it’s cheap but not to use it because it’s garbage? That’s not advice, that’s a riddle. And why are we all acting like foot care is some secret ritual? My grandma did this in the 70s. We’re overcomplicating the hell out of a simple thing: check your feet, don’t burn them, don’t walk barefoot. And if your doctor’s not listening? Find a new one. Simple.
Rachelle Baxter
November 30, 2025 AT 17:34First: you must wear diabetic socks. Not ‘socks that say diabetic on them.’ Actual medical-grade, seamless, non-constricting, moisture-wicking socks. Second: never use a heating pad. Ever. Third: duloxetine is not ‘just an antidepressant’-it’s an SNRI with proven neuro-modulating effects. Fourth: if you’re using NSAIDs, you’re risking renal failure. Fifth: your doctor is not your friend. They’re a gatekeeper. Sixth: Medicare covers custom orthotics-ask for them. Seventh: your foot ulcer isn’t ‘just a sore.’ It’s a medical emergency. Eighth: stop Googling ‘natural cures.’ Ninth: your pain is real. Tenth: you deserve to live without fear. Eleventh: I’m not your mom, but I’m watching.
Dirk Bradley
December 2, 2025 AT 11:11While the clinical efficacy of duloxetine and pregabalin has been demonstrated in randomized controlled trials with a mean reduction in pain scores of 37.2% (95% CI: 32.1–42.3), one must remain cognizant of the pharmacoeconomic implications of long-term administration. The capsaicin patch, while efficacious, necessitates a clinical setting and incurs significant procedural costs. Moreover, the adherence to daily foot inspection protocols remains suboptimal in 68% of the diabetic population according to CDC 2023 surveillance data. One must therefore prioritize evidence-based interventions over anecdotal narratives, however emotionally compelling.
Emma Hanna
December 3, 2025 AT 06:20Wait. You said ‘never go barefoot’-but you didn’t capitalize ‘Never.’ That’s sloppy. And you wrote ‘lukewarm’ without a hyphen? That’s not even a word in proper usage. And you said ‘meds’? That’s slang. This post is full of errors. If you’re going to give medical advice, at least use proper grammar. Also, gabapentin isn’t FDA-approved for this? Then why are you recommending it? You’re misleading people. This is dangerous.
Mariam Kamish
December 4, 2025 AT 08:57Yeah right. Like anyone’s gonna do all that foot stuff. I’ve got kids, a job, and a cat that knocks over my socks. Who has time? And duloxetine made me feel like a zombie. I’d rather just live with the pain. At least it’s mine.
Patrick Goodall
December 6, 2025 AT 01:55They’re hiding the real solution. It’s not the meds, it’s the EMF from cell phones and Wi-Fi frying your nerves. I read a study from a guy in Sweden who cured his neuropathy by wrapping his feet in aluminum foil and sleeping in a Faraday cage. No joke. The FDA banned his research. You think they want you walking? Think again. I’ve got a video of me walking barefoot on ice after 6 months of foil therapy. It’s on YouTube. Search ‘Neurofoil King.’