When you take a pill, injection, or inhaler, you expect it to work exactly as it should - not weaker, not stronger, not broken down by heat or humidity. That’s not luck. It’s the result of stability testing, a rigid, science-backed process that tracks how drugs hold up over time under real-world conditions. This isn’t optional. If a drug degrades and loses potency, patients don’t get the treatment they need. Worse, degradation can create harmful byproducts. That’s why regulators demand precise, repeatable stability testing protocols - especially around temperature and time.
Why Temperature and Time Matter More Than You Think
Drugs aren’t static. They react. Heat, moisture, and even light can change their chemical structure. A tablet stored in a hot car for a week might lose 10% of its active ingredient. A liquid vaccine left at room temperature too long could clump and become ineffective. Stability testing answers one simple question: How long can this product stay safe and effective under real storage conditions?
The answer isn’t guessed. It’s measured. And it starts with standardized conditions set by the International Council for Harmonisation (ICH). Since 2003, ICH Q1A(R2) has been the global rulebook for stability testing. It’s followed by the FDA, EMA, Health Canada, and nearly every major regulator. This isn’t about bureaucracy - it’s about consistency. If a drug works in Melbourne, it must work in Mumbai, Berlin, or Toronto. The same temperature and time rules apply everywhere.
The Three Core Testing Conditions
Stability testing isn’t one test. It’s three layered tests, each with strict temperature and humidity targets. These aren’t suggestions - they’re mandatory.
- Accelerated Testing: 40°C ± 2°C and 75% RH ± 5% RH for 6 months. This isn’t meant to mimic real life. It’s a stress test. If a drug fails here, it’s unlikely to last a year in normal storage. This condition was chosen because it’s hot enough to speed up degradation without melting common excipients - a detail FDA scientists confirmed in 2022.
- Long-Term Testing: Two options. Either 25°C ± 2°C and 60% RH ± 5% RH, or 30°C ± 2°C and 65% RH ± 5% RH. The choice depends on where the product will be sold. Most companies pick 25°C/60% RH for global markets, but if you’re targeting tropical regions (Zone IVa), you must test at 30°C/65% RH. Data must cover at least 12 months at submission, according to FDA guidelines.
- Intermediate Testing: 30°C ± 2°C and 65% RH ± 5% RH for 6 months. This is only required if the long-term test is done at 25°C and the accelerated test shows signs of change. It’s a bridge - a way to confirm that the drug won’t degrade faster than expected under moderate heat.
For refrigerated products - like many biologics and vaccines - the rules shift. Long-term storage is at 5°C ± 3°C for 12 months. Accelerated testing jumps to 25°C ± 2°C and 60% RH, not 40°C. Why? Because freezing and thawing, not heat, are the real threats here. WHO guidelines make this clear, and ignoring it has led to recalls.
How Long Do You Really Have to Test?
Time isn’t just a number. It’s a commitment. For long-term testing, you need a minimum of 12 months of data to file for approval. But most studies run much longer - 24, 36, even 48 months - to establish a full shelf life. The testing schedule is tight: samples are pulled at 0, 3, 6, 9, 12, 18, 24, and 36 months. Early time points catch fast-degrading products. Later ones prove long-term stability.
Here’s the catch: you can’t rush it. Even with accelerated data, regulators won’t approve a 3-year shelf life based on 6 months of real-time testing. The correlation between accelerated and real-time results is strong - about 85% for small molecules - but it fails for hygroscopic drugs, biologics, or complex formulations. That’s why you can’t skip the long-term test.
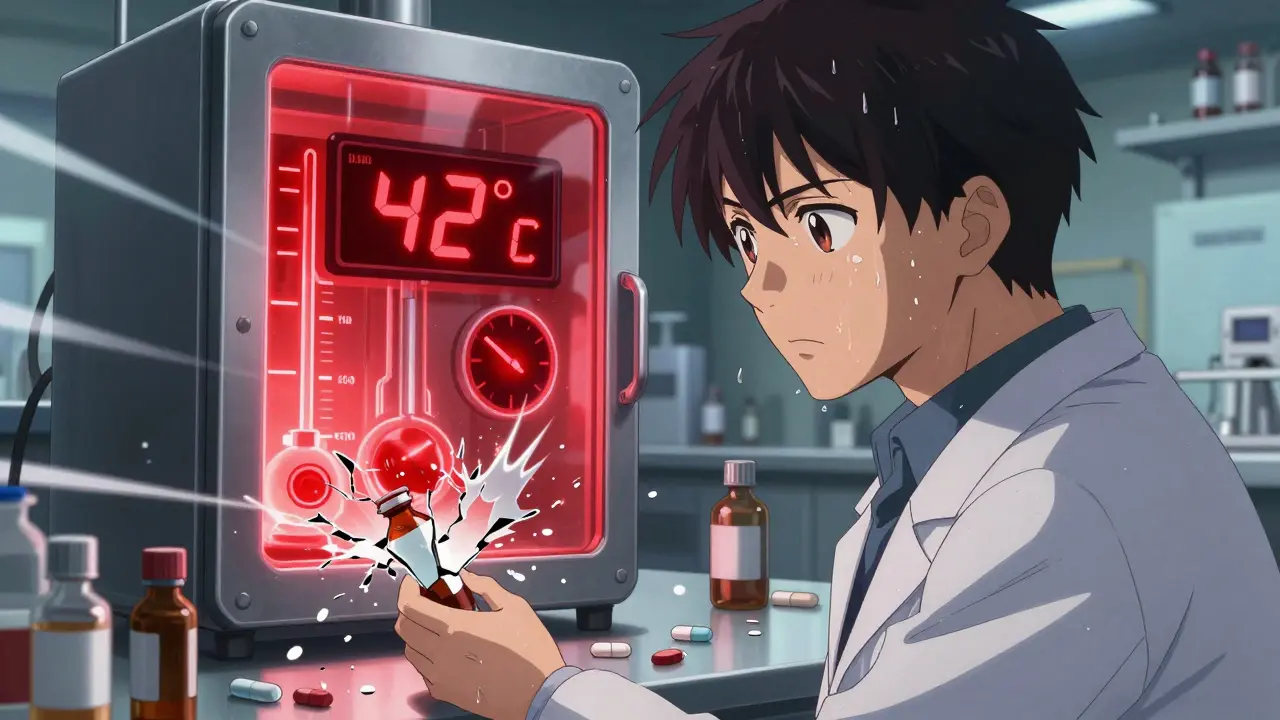
And you can’t fake the data. Stability chambers must hold temperature within ±0.5°C and humidity within ±2% RH. If a chamber spikes to 42°C for two hours during a 6-month study? The entire run is invalid. A 2023 LinkedIn survey of 142 professionals found that 78% had experienced at least one temperature excursion that ruined a study. One slip can cost months - and millions.

Global Differences and Hidden Traps
ICH harmonized testing globally - but not perfectly. The FDA requires 12 months of long-term data at submission. The EMA lets you submit with only 6 months if you’re using Option B. That sounds like flexibility. In practice, it’s a delay. Companies filing in both regions often end up running two parallel studies, just to meet each agency’s requirement.
Then there’s climate zones. ICH defines five. Zone I (Temperate) uses 21°C/45% RH. Zone IVb (Hot/Higher Humidity) uses 30°C/75% RH. If your drug is meant for Southeast Asia, you can’t just test at 25°C. You need a separate study at 30°C/75% RH. Tovatech’s 2023 survey found this adds 4 to 6 months to development timelines. For generics, that’s a huge financial hit.
And then there’s the gray zone: “significant change.” ICH Q1A(R2) says a product fails if there’s a 5% change in assay, degradation products exceed thresholds, or physical properties like color or texture change. But it doesn’t define what “significant” means statistically. A Pfizer quality analyst shared a case where a 4.8% drop in potency - within normal statistical variation - was flagged as a failure. Regulators saw a red flag. The company had to run extra tests, delay launch, and spend $200,000 on additional validation.
What Happens When It Goes Wrong?
Failure isn’t theoretical. In 2021, Teva recalled 150,000 vials of Copaxone® after stability tests at 40°C revealed protein aggregation. The drug was safe, but potency dropped. Patients got weaker doses. In 2022, the FDA issued 27 warning letters citing stability testing flaws - one of the top reasons for regulatory action.
Biologics are especially vulnerable. Monoclonal antibodies, mRNA vaccines, and cell therapies degrade in ways standard tests don’t catch. Freeze-thaw cycles, agitation, even container materials can break them down. FDA warning letters to Amgen and Roche in 2021 and 2022 pointed to exactly this. The ICH guidelines were written for pills and syrups. They weren’t built for living molecules.

How Companies Are Adapting
Smart companies aren’t just following the rules - they’re pushing beyond them. Merck used intermediate testing at 30°C/65% RH to catch a polymorphic transition in Keytruda® - a hidden change in crystal structure that could’ve affected absorption in tropical climates. They fixed it before launch.
Others are turning to predictive modeling. Over 70% of top pharma firms now run accelerated studies at 50°C to 80°C to predict degradation faster. These “APS” studies can cut time-to-market by 9 to 12 months. But regulators are skeptical. The EMA rejected 8 model-based submissions in 2022-2023 because they didn’t meet the bar for validation.
Real-time testing is the future. The FDA’s 2023 pilot program uses process analytical technology (PAT) to monitor drug quality during manufacturing - not after. If a tablet’s hardness, moisture, and composition are tracked continuously, maybe you don’t need to wait 12 months to prove stability. Early results show a 30-50% reduction in required testing. But it’s still experimental.
What You Need to Get Started
If you’re developing a drug, here’s your checklist:
- Choose your long-term condition based on target markets (25°C/60% RH for global, 30°C/65% RH for tropical).
- Run accelerated testing at 40°C/75% RH for 6 months - no exceptions.
- Set up chambers with ±0.5°C and ±2% RH control. Use dual-loop systems if humidity is unstable.
- Map your chamber. Temperature varies by shelf. Document every hotspot and cold spot.
- Test at 0, 3, 6, 9, 12, 18, 24, 36 months. More often if degradation is expected.
- Define “significant change” in your protocol - and justify it with statistics.
- Archive all raw data. A typical stability dossier runs 450-600 pages.
Training takes 6-9 months. You need to understand ANOVA, regression, environmental controls, and regulatory writing. The job is repetitive, but it’s critical. One analyst told us: “If you mess this up, someone doesn’t get their medicine. That’s heavier than any deadline.”
The Bottom Line
Stability testing isn’t about checking a box. It’s about protecting lives. The temperature and time conditions aren’t arbitrary. They’re based on decades of data, real-world failures, and hard lessons. ICH Q1A(R2) may be 20 years old, but it still works - for now. The next update, expected in late 2024, will address biologics, nanoparticles, and continuous manufacturing. Until then, the rules are clear: test at the right temperature, at the right time, with the right precision. There’s no shortcut. And there shouldn’t be.
What are the standard temperature and humidity conditions for long-term stability testing?
The ICH Q1A(R2) guidelines define two standard conditions for long-term stability testing: 25°C ± 2°C with 60% RH ± 5% RH, or 30°C ± 2°C with 65% RH ± 5% RH. The choice depends on the target market’s climate zone. For global products, 25°C/60% RH is most common. For tropical markets (Zone IVa), 30°C/65% RH is required. Data must cover at least 12 months for regulatory submission.
Why is accelerated testing done at 40°C and 75% RH?
The 40°C/75% RH condition was chosen to simulate extreme but realistic environmental stress - like a drug package left in a hot warehouse or during shipping. It’s hot enough to accelerate degradation without melting excipients or causing non-representative reactions. Studies show this condition correlates to about 24 months of real-time stability at 25°C/60% RH for 85% of small molecule drugs, making it a reliable predictor.
Can I use predictive modeling instead of real-time stability testing?
Some companies use predictive models with higher temperatures (50-80°C) to estimate shelf life faster. These are called Accelerated Predictive Stability (APS) studies. While 74% of top pharma firms use them, regulators like the EMA still require real-time data for approval. Model-based submissions were rejected 8 times by the EMA between 2022 and 2023. Predictive models are useful for internal decisions but aren’t yet accepted as full replacements for ICH-compliant testing.
What happens if my stability chamber has a temperature excursion?
A temperature excursion - even a brief one - can invalidate your entire stability study. Regulators require chambers to maintain ±0.5°C. If a chamber spikes to 42°C for a few hours, the data from that period is no longer reliable. You must document the event, investigate the cause, and often repeat the study. In a 2023 survey, 78% of professionals reported at least one excursion that caused study failure.
Do refrigerated products follow the same stability rules?
No. Refrigerated products - like vaccines and biologics - are tested at 5°C ± 3°C for long-term storage. Their accelerated condition is 25°C ± 2°C and 60% RH, not 40°C. This is because freezing, thawing, and agitation are bigger threats than heat. Testing at 40°C would cause irreversible damage and give false results. WHO Annex 10 and FDA guidance both specify these adjusted conditions for cold-chain products.
How long does a typical stability study take to complete?
A full long-term stability study takes at least 12 months to reach submission, but most run for 24 to 36 months to establish a full shelf life. Accelerated testing takes 6 months. Intermediate testing, if needed, adds another 6 months. The waiting period is a major bottleneck - 67% of companies report delays in product launch due to stability data not being ready on time.





Joni O
January 19, 2026 AT 05:25This post literally saved my sanity last quarter when our stability chamber had a 3-hour spike. I thought we were done for. Turns out, documenting the excursion and running a root cause analysis actually impressed the auditor. Just remember: it’s not the error, it’s how you fix it. 🙌
Ryan Otto
January 19, 2026 AT 11:07Let’s be honest - ICH Q1A(R2) is a relic. The 40°C/75% RH condition was derived from 1990s pharmaceutical logistics, not modern supply chains. We’re still using analog protocols for digital-age molecules. The fact that regulators still treat biologics like aspirin is not just outdated - it’s dangerous. And don’t get me started on the 5% degradation threshold - statistically meaningless when your assay has a 2% RSD.
Max Sinclair
January 19, 2026 AT 23:25Great breakdown. I especially appreciate how you highlighted the difference between global and tropical zones - too many teams assume one size fits all. Also, the note about chamber mapping? Absolute gold. I’ve seen so many studies get tossed because someone didn’t check the top shelf. Pro tip: use thermal imaging before you even load samples. Saves weeks.
Andrew McLarren
January 20, 2026 AT 19:43While the regulatory framework is indeed robust, it is imperative to acknowledge the growing disparity between the empirical requirements of traditional small-molecule drugs and the dynamic instability profiles of biologics. The current ICH guidelines, though historically sound, lack the granularity required to adequately characterize conformational degradation pathways, particularly in lyophilized formulations subjected to mechanical stress during transit. A paradigm shift toward real-time, in-situ monitoring is not merely advantageous - it is an ethical imperative.
Andrew Short
January 21, 2026 AT 13:15Anyone who thinks predictive modeling is the future is either delusional or on a pharma payroll. The EMA rejected 8 submissions because they were garbage. You can’t replace real-time data with math magic. And those companies running 80°C studies? They’re not innovating - they’re cutting corners and gambling with patient lives. Wake up. This isn’t Silicon Valley. Lives are on the line.
christian Espinola
January 23, 2026 AT 10:5478% of professionals had a chamber excursion? That’s not coincidence. That’s systemic failure. Who’s really controlling these chambers? The same people who signed off on the SOPs written by interns? And why is the FDA still accepting 12-month data for 3-year shelf life? They’re letting companies extrapolate like it’s a math test. This isn’t science - it’s a confidence game.
Chuck Dickson
January 24, 2026 AT 01:26Big thanks for this - seriously. I’m new to stability testing and this felt like someone finally explained it without jargon soup. I used to think it was just ‘stick it in a box and wait.’ Now I get why we map shelves, why we archive every single data point, and why that one 0.3°C fluctuation matters. Also - yes, the 5% rule is wild. My team just had a 4.9% drop flagged. We had to redo three months of work. 😅 But now I get it. This stuff is sacred.
Robert Cassidy
January 24, 2026 AT 22:33They want us to test at 30°C/65% RH for tropical markets? That’s a joke. Those countries can’t even keep their power grid stable. The whole system is rigged - big pharma gets to run perfect labs in Ohio while patients in Nigeria get degraded meds because the local clinic has no AC. This isn’t science - it’s colonialism with a lab coat. And don’t tell me about ‘global standards’ - standards for who? For the WHO? For the FDA? Not for the people who need the medicine.
Naomi Keyes
January 25, 2026 AT 15:45Actually, I must correct you - the ICH Q1A(R2) guideline does not specify that the 25°C/60% RH condition is "most common" - it specifies that it is the "default condition" for Zone I, and that "alternative conditions" may be used based on climate zone. Furthermore, the "at least 12 months" requirement applies only to submission, not to the full study duration - which, as you correctly noted, often extends to 36 or 48 months. Also - you mentioned "dual-loop systems" - but did you mean "dual-loop temperature control systems" or "dual-loop humidity control systems"? Precision matters.
Dayanara Villafuerte
January 26, 2026 AT 08:51My cousin works in a rural clinic in Colombia. They once got a batch of insulin that was "within specs" on paper - but the fridge broke for 18 hours during transport. The vials were fine, but the patients? Not so much. 🥲 This post? 10/10. If every regulator read this, maybe we’d stop treating medicine like a spreadsheet.