Strep throat isn’t just a sore throat. It’s a bacterial infection that can turn mild discomfort into something serious if left untreated. Unlike a cold or the flu, strep throat doesn’t come with a runny nose or cough. Instead, it hits hard and fast-sudden pain when swallowing, fever, swollen tonsils with white patches, and tender lymph nodes in the neck. If you’ve had this before, you know how quickly it can knock you out. And if you’ve got kids, you’ve probably seen it sweep through schools and daycares like wildfire.
How Do You Know It’s Strep and Not Just a Virus?
The biggest mistake people make is assuming every sore throat is strep. About 80% of sore throats are viral-caused by colds, flu, or even allergies. But strep throat, caused by Group A Streptococcus (a bacterium called Streptococcus pyogenes), behaves differently. It doesn’t come with sneezing, watery eyes, or congestion. In fact, if you have a cough, it’s probably not strep. That’s one of the most reliable clues.
Doctors use a simple scoring system called the Centor criteria (a clinical tool that assigns points for fever, absence of cough, swollen lymph nodes, and tonsil exudate). If you score 3 or more points, testing is recommended. For kids, the threshold is even lower-any sudden throat pain with fever and no cough is a red flag. Adults are less likely to get it, but when they do, it’s often more severe.
Here’s what to look for:
- Sudden, severe throat pain (95% of cases)
- Fever above 100.4°F (38°C) (85% of cases)
- White patches or pus on tonsils (70% of cases)
- Tender, swollen lymph nodes in the neck (60% of cases)
- Small red spots on the roof of the mouth (palatal petechiae)-rare, but very specific
- No cough, no runny nose, no hoarseness
That last point matters. If you’ve got a cough, you’re likely dealing with a virus. Strep throat is quiet in the nose and lungs-it’s all about the throat.
How Is Strep Throat Actually Diagnosed?
You can’t tell strep just by looking. You need a test. There are three main options, each with pros and cons.
The rapid antigen detection test (RADT) (a throat swab that detects strep bacteria in minutes) is the most common. It’s fast-results in 10 to 30 minutes-and highly accurate for ruling strep in. If it’s positive, you’ve got it. But here’s the catch: it can miss up to 15% of cases, especially in kids under 5. That’s why, if your child tests negative but still looks like they have strep, doctors often follow up with a culture.
The throat culture (a swab sent to a lab to grow the bacteria) is the gold standard. It takes 24 to 48 hours, but it catches almost all cases-90% to 95% sensitivity. It’s the go-to for kids and teens because untreated strep can lead to rheumatic fever, a serious heart condition.
A newer option is PCR molecular testing (a DNA-based test that detects bacterial genes). It’s more sensitive than the rapid test-95% to 98% accurate-and results come in 24 to 48 hours. It’s becoming more common in urgent care centers and hospitals, especially where accuracy is critical.
In 2024, the FDA approved a new test called Strep Ultra (a rapid molecular test with 98% sensitivity and 15-minute results). It’s starting to replace older rapid tests in clinics that can afford it. For now, though, most offices still use the quick swab.
Adults with low Centor scores and negative rapid tests often don’t need further testing. But for kids? Always confirm. The stakes are higher.

Which Antibiotics Are Used-and Which Ones Actually Work?
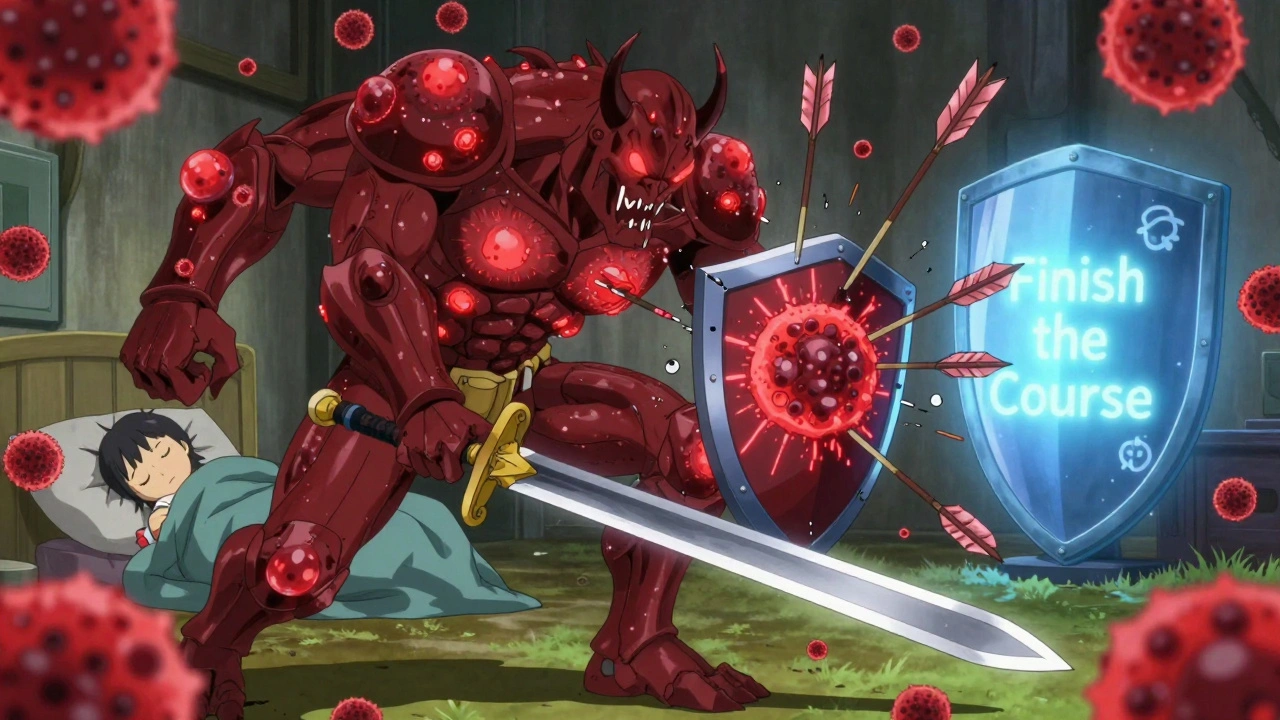
Antibiotics aren’t just to feel better faster. They prevent complications. The biggest danger? rheumatic fever (a condition where the immune system attacks the heart, joints, and brain after untreated strep). It affects about 3% of untreated cases. In children, it can lead to lifelong heart damage.
First-line treatment? Penicillin V (an oral antibiotic taken twice daily for 10 days) or amoxicillin (a more palatable option, especially for kids, taken once or twice daily). Both are cheap, effective, and have been used for over 70 years. They clear the infection in 95% of cases.
For people allergic to penicillin, options include:
- Cephalexin (a first-generation cephalosporin, taken twice daily)
- Clindamycin (used when resistance is suspected, taken three times daily)
- Azithromycin (a 5-day course, but less effective-only 85-90% success rate)
Here’s the hard truth: macrolide resistance (resistance to azithromycin and similar drugs) is rising. In some areas, up to 15% of strep strains don’t respond. That’s why guidelines now recommend penicillin first-even if it’s not the most convenient.
Cost-wise, generic penicillin V runs about $4 for a full 10-day course. Azithromycin? Up to $250 if you don’t have insurance. That’s not just about money-it’s about effectiveness.
And here’s something most people don’t realize: antibiotics don’t make you feel better instantly. They reduce symptoms by about 16 hours on average. That’s not a lot. But they stop you from spreading it to others-and that’s the real win.
What’s the Real Recovery Timeline?
If you start antibiotics within 48 hours of symptoms, you’ll feel better in 24 to 48 hours. The fever drops. Swallowing gets easier. The white patches fade. But feeling better doesn’t mean you’re done.
Here’s what to expect:
- Day 1: Symptoms peak. Fever, pain, fatigue. Start antibiotics.
- Day 2-3: Fever breaks. Throat pain improves by 50%. You can start eating soft foods.
- Day 4-5: Most symptoms gone. You’re no longer contagious after 24 hours of antibiotics, as long as fever is gone.
- Day 7-10: Full recovery. Tonsils return to normal. No more fatigue.
Without antibiotics? Symptoms last 7 to 10 days, and you’re contagious the whole time. That’s why schools and workplaces require you to stay home for 24 hours after starting antibiotics.
Don’t stop the antibiotics just because you feel better. About 40% of parents quit early when symptoms improve. That’s dangerous. Incomplete treatment leads to relapse in 5% to 15% of cases-and increases the risk of rheumatic fever.
And here’s a hidden risk: peritonsillar abscess (a pus-filled pocket behind the tonsil). It happens in 1% to 2% of cases, usually when treatment is delayed. Symptoms include one-sided throat pain, muffled voice, trouble opening the mouth, and drooling. If you’ve been on antibiotics for 48 hours and you’re getting worse, go back. This needs drainage.
What Not to Do (And What Really Works)
People make the same mistakes over and over.
Don’t share antibiotics. A 2024 Reddit survey found 8% of adults have given leftover antibiotics to family members. That’s not just wrong-it’s dangerous. Dosing is based on weight and age. Giving your kid your azithromycin could lead to underdosing and resistance.
Don’t use leftover antibiotics. CDC surveys show 12% of people keep antibiotics for "next time." But strep doesn’t always come back the same way. Using old meds can mask symptoms and make future infections harder to treat.
Do rest. Your body needs energy to heal. Don’t push through school or work. Even after 24 hours, fatigue can linger.
Do stay hydrated. Swallowing hurts. Sip cold water, suck on ice chips, or try popsicles. Warm broth helps too. Avoid citrus-it stings.
Do finish the full course. This isn’t a suggestion. It’s medical law. 95% of people who finish their antibiotics fully clear the infection. Those who don’t? They’re the ones who end up back in the clinic.
When to Call the Doctor Again
Most cases resolve without issue. But watch for these red flags:
- Fever returns after 48 hours of antibiotics
- Difficulty breathing or swallowing
- Swelling in the neck or jaw
- Joint pain, rash, or swelling in the knees or ankles
- Dark urine or swelling in the face or legs (signs of kidney inflammation)
These could mean complications like rheumatic fever, kidney inflammation (post-streptococcal glomerulonephritis), or abscess. Don’t wait. Call your doctor or go to urgent care.
And if you’ve had strep twice in a year? You might be a carrier-someone who harbors the bacteria without symptoms. That’s rare, but it happens. A specialist may need to check for hidden infection in the tonsils or sinuses.
Strep throat isn’t glamorous. But it’s common, dangerous if ignored, and easy to treat-if you do it right. The key isn’t fancy medicine. It’s knowing when to test, which antibiotic to take, and having the discipline to finish it. That’s how you protect yourself, your kids, and your community from something that can change lives forever.
Can you get strep throat without a fever?
Yes, but it’s rare. Fever is present in about 85% of confirmed cases. If you have severe throat pain, white patches, and swollen lymph nodes but no fever, it’s still possible to have strep-especially in older adults or people with weakened immune systems. Testing is still recommended if other symptoms match.
Is strep throat contagious after 24 hours of antibiotics?
No. Once you’ve been on antibiotics for 24 hours and your fever is gone, you’re no longer contagious. That’s why most schools and workplaces allow you to return after one full day of treatment. But keep washing your hands and avoid sharing cups or utensils for a few more days.
Can you test negative for strep and still have it?
Yes. Rapid tests miss 5% to 15% of cases, especially in young children. If symptoms are strong and the rapid test is negative, a throat culture is needed to confirm. Don’t rely on a negative rapid test alone-especially in kids.
Why is penicillin still the first choice for strep throat?
Because it’s cheap, effective, and resistance is extremely rare-only about 0.5% of Group A strep strains are resistant. Newer antibiotics like azithromycin are more expensive and have higher resistance rates. Penicillin has been used for decades and still works better than anything else for strep throat.
Can strep throat come back after treatment?
Yes, but not because the antibiotic failed. Relapse usually happens if the full 10-day course wasn’t finished. It can also happen if you’re exposed again-strep spreads easily. In rare cases, someone becomes a carrier and re-infects themselves or others. If you get strep twice in a year, talk to your doctor about possible underlying causes.
Are there any home remedies that help with strep throat?
Saltwater gargles, honey in tea, and cold liquids can ease discomfort, but they don’t kill the bacteria. Only antibiotics do that. Don’t use essential oils, apple cider vinegar, or garlic as substitutes-they’re not proven and can delay proper treatment. Home remedies help you feel better, but they don’t replace medicine.
Can adults get strep throat from kids?
Absolutely. Strep spreads through droplets-coughing, sneezing, sharing utensils. Adults are less likely to get it than kids, but when they do, it’s often more severe. Parents and teachers are at higher risk. Wash hands often, especially after helping a sick child.
Is there a vaccine for strep throat?
Not yet. Researchers have been trying for decades. The bacteria has over 200 different strains, and the protein it uses to hide from the immune system (M-protein) changes too much to target with one vaccine. Several candidates are in early trials, but none are close to being available. For now, prevention means good hygiene and prompt treatment.





Inna Borovik
December 7, 2025 AT 07:55Let’s be real-most people don’t know the difference between a viral sore throat and strep, and they panic over a sniffle. The Centor criteria exists for a reason. Skip the Google diagnosis. Get tested. Penicillin isn’t glamorous, but it’s the only thing that actually works without breeding superbugs. Stop treating antibiotics like candy.
Andrew Frazier
December 8, 2025 AT 22:56USA still uses penicillin?? Bro we got better stuff now. Azithromycin is way easier-once a day, no big deal. Why are we stuck in the 1950s? This is 2024. I got my kid on Z-Pak last year and he was back on the soccer field in 2 days. Penicillin? That’s what your grandpa took.
Dan Cole
December 9, 2025 AT 20:06You think penicillin is outdated? Let me break this down for you, Andrew. Resistance isn’t a myth-it’s a mathematical inevitability when you misuse antibiotics. Azithromycin has a 15% failure rate in some regions. Penicillin? 0.5%. That’s not tradition-it’s evolution. You don’t upgrade a hammer because it’s "old," you upgrade it when it breaks. And penicillin hasn’t broken. It’s the only antibiotic that doesn’t give Streptococcus pyogenes a chance to evolve around it. The fact that you’d rather trust a 5-day course of a drug with 10x the cost and half the reliability says more about your priorities than your medical knowledge.
And don’t even get me started on people giving leftover antibiotics to their kids. That’s not parenting. That’s biological roulette. You’re not saving money-you’re creating a superbug that’ll kill someone’s grandkid in 2030.
Modern medicine isn’t about convenience. It’s about precision. And if you can’t grasp that, you shouldn’t be making medical decisions for anyone but yourself.
Karen Mitchell
December 10, 2025 AT 11:03It’s deeply concerning that this post normalizes the medicalization of every sore throat. Why are we so quick to reach for antibiotics? What about the microbiome? What about immune resilience? We’ve turned a minor, self-limiting illness into a pharmaceutical emergency. This isn’t healthcare-it’s fear-based consumerism. And now parents are terrified of a fever. The real epidemic is our collective abandonment of natural healing.
Mayur Panchamia
December 11, 2025 AT 13:57Listen here, Karen-you sound like someone who thinks honey cures cancer! Strep throat isn’t "a minor illness"-it’s a ticking time bomb that can destroy your heart! Rheumatic fever doesn’t care if you believe in crystals or tea! If your kid has white patches and no cough, you don’t sit there and "let it run its course"-you get that swabbed! And if you’re too lazy to drive to the clinic, then don’t complain when your kid ends up with a hole in his heart! Penicillin is $4! Azithromycin is $250! Who’s the real villain here? The doctor who prescribes it-or you, who’d rather gamble with your child’s life because you hate pills?
brenda olvera
December 12, 2025 AT 11:51My cousin in Mumbai got strep last year and they just gave her turmeric milk and rest. She felt better in 3 days. Maybe we don’t need antibiotics for everything? I know it’s scary, but maybe our bodies can handle more than we think? Let’s not rush to the pharmacy every time we feel a little sore.
Geraldine Trainer-Cooper
December 13, 2025 AT 05:40penicillin is the only thing that works. period. no debate. azithromycin is for people who don’t want to take meds twice a day. and yes i know what resistance is. i’ve seen it. in the wild. in the clinic. in my own family. stop the nonsense.
olive ashley
December 14, 2025 AT 10:55Did you know the CDC is quietly phasing out rapid strep tests in favor of PCR? They’ve known for years the old tests miss too many cases. And now they’re pushing the new Strep Ultra test-98% accurate-but only in hospitals. Why? Because they don’t want parents to know how often the $10 rapid test fails. It’s all about cost control. They’d rather you get rheumatic fever than spend $20 on a better test. Wake up.
Rashmi Gupta
December 15, 2025 AT 06:09Actually, in India, we’ve had a 70% drop in strep cases since 2020-not because of antibiotics, but because of mask-wearing and handwashing. Maybe the real solution isn’t drugs, but hygiene? Why are we still treating this like a 1940s problem when we have 21st-century tools? The entire Western medical model is broken.
Dan Cole
December 15, 2025 AT 16:33So your solution to strep throat is… masks? That’s rich. Masks stopped flu transmission, yes-but strep is spread by direct contact, not airborne droplets. You wipe your nose, touch a doorknob, your kid touches it, then puts their hand in their mouth. That’s how it spreads. A mask doesn’t stop that. And if you think hygiene alone prevented strep, then why did rheumatic fever rates spike in rural India during the pandemic? Because people couldn’t get to clinics. No antibiotics. No testing. Just hope. And now we have kids with damaged heart valves because someone thought "natural immunity" was a better plan than penicillin. Your logic is charming. It’s also dead wrong.