Antihistamine Safety Checker for Older Adults
Is Your Antihistamine Safe?
Select your antihistamine to see its fall risk compared to safer alternatives for older adults.
Safety Assessment
Safety Rating
Recommendation
Why Sedating Antihistamines Are a Hidden Danger for Older Adults
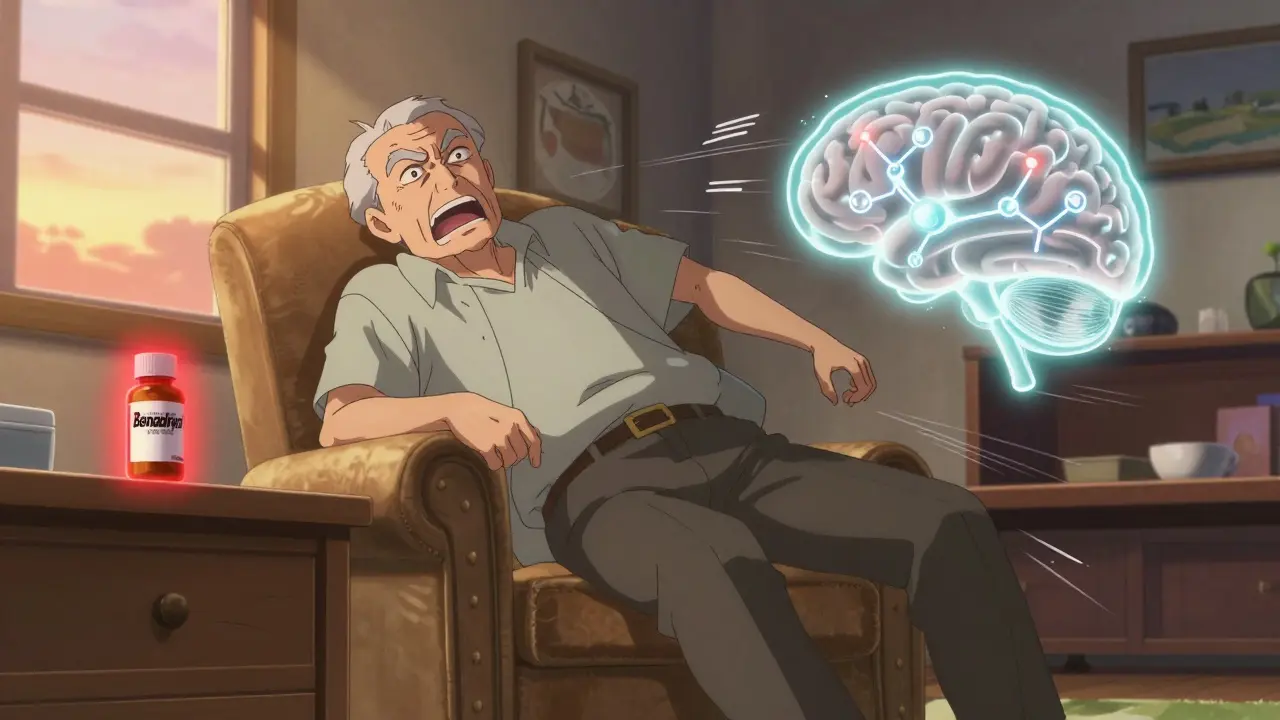
Every year, more than one in four adults over 65 falls. Many of these falls aren’t just accidents-they’re linked to medications people think are harmless. One of the biggest culprits? First-generation antihistamines like diphenhydramine (Benadryl), chlorpheniramine, and brompheniramine. These drugs are sold over the counter as sleep aids, allergy relievers, or cold remedies. But for older adults, they’re not safe. They don’t just stop sneezing-they slow down the brain, blur vision, throw off balance, and turn a simple walk to the bathroom into a life-threatening event.
Unlike newer antihistamines, these older drugs easily cross into the brain. That’s how they cause drowsiness. But in someone over 65, the body processes them slower. A 25mg dose of diphenhydramine might wear off in 6 hours for a 30-year-old. For a 75-year-old, it can linger for 12 hours or more. That means dizziness and unsteadiness aren’t just a side effect-they’re a prolonged state. And when you’re already at risk for falls due to weak muscles, poor vision, or balance issues, that extra drowsiness is enough to send you tumbling.
The Numbers Don’t Lie: How Much Risk Are We Talking About?
A 2025 study of nearly 200,000 older adults found that those who filled a prescription for a first-generation antihistamine had an 8% chance of falling and needing medical care within 60 days. That’s not a small number. It’s not a rare event. It’s a predictable outcome.
Another study, published in Osteoporosis International, looked at over 10,000 older adults and found they were 54% more likely to suffer an injurious fall-and 43% more likely to break a bone-if they took these medications. That’s not a slight increase. That’s a major spike. And it’s not just falls. Hospital records show older adults on diphenhydramine are more than twice as likely to develop delirium, a sudden, dangerous confusion that makes them disoriented, agitated, and even more prone to falling.
The American Geriatric Society has labeled these drugs as “potentially inappropriate” for seniors. That’s their strongest warning. They’re on the Beers Criteria list-the official list of medications doctors should avoid prescribing to older adults. Yet, they’re still sold everywhere: drugstores, grocery stores, online. No prescription needed. No warning big enough to make people pause.
First-Generation vs. Second-Generation: The Clear Difference
Not all antihistamines are the same. The newer ones-loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra)-were designed to stay out of the brain. They block histamine where it causes allergies (in the nose, throat, skin), not where it causes drowsiness (in the brain).
Here’s the breakdown:
| Antihistamine | Generation | Common Brand | Drowsiness Risk | Anticholinergic Burden | Fall Risk Increase |
|---|---|---|---|---|---|
| Diphenhydramine | First | Benadryl | 15-20% | 3-4 (High) | +87% |
| Chlorpheniramine | First | Chlor-Trimeton | 12-18% | 3-4 (High) | +80% |
| Cetirizine | Second | Zyrtec | 14% | 1 (Low) | +4% |
| Loratadine | Second | Claritin | 6% | 0 (None) | No increase |
| Fexofenadine | Second | Allegra | 5% | 0 (None) | No increase |
The data is clear: fexofenadine and loratadine don’t raise fall risk. Cetirizine has a slight risk, but it’s far lower than the first-generation drugs. If you need an antihistamine, these are the only safe choices for older adults.
Why Are These Dangerous Drugs Still So Common?
Here’s the uncomfortable truth: doctors still prescribe them. Pharmacists still sell them. And older adults still take them-often without knowing why.
In 2024, diphenhydramine was the third most popular over-the-counter sleep aid sold to Americans over 65. Over 28 million doses were bought. That’s not just a few people. That’s millions. And the labels? They say “may cause drowsiness.” That’s it. No bold warning. No mention of falls. No reference to dementia risk or delirium.
Even worse, studies show doctors prescribe these drugs at the same rate to older and younger patients. A dermatologist treating a 70-year-old with hives is just as likely to write for diphenhydramine as they are for a 25-year-old. But the risks? They’re not the same. A 70-year-old doesn’t just feel sleepy-they become unsteady. Their reaction time slows. Their balance fails. And if they’ve had a fall before? The risk multiplies.

What to Do: Three Simple Steps to Stay Safe
- STOP first-generation antihistamines immediately if you’re over 65. That means no Benadryl for sleep. No Dimetapp for colds. No generic “nighttime allergy” pills. Check the ingredient list. If it says diphenhydramine, chlorpheniramine, or brompheniramine-don’t take it.
- SWITCH to a second-generation antihistamine. Fexofenadine (Allegra) is the safest. Loratadine (Claritin) is next. Cetirizine (Zyrtec) is okay if you’re careful, but avoid it if you’re already dizzy or have balance issues.
- REDUCE all other sedating meds at the same time. If you’re taking a benzodiazepine, an opioid, or a sleeping pill, talk to your doctor about cutting back. These drugs multiply the danger. Taking diphenhydramine and sleeping pills together? That’s a recipe for a fall.
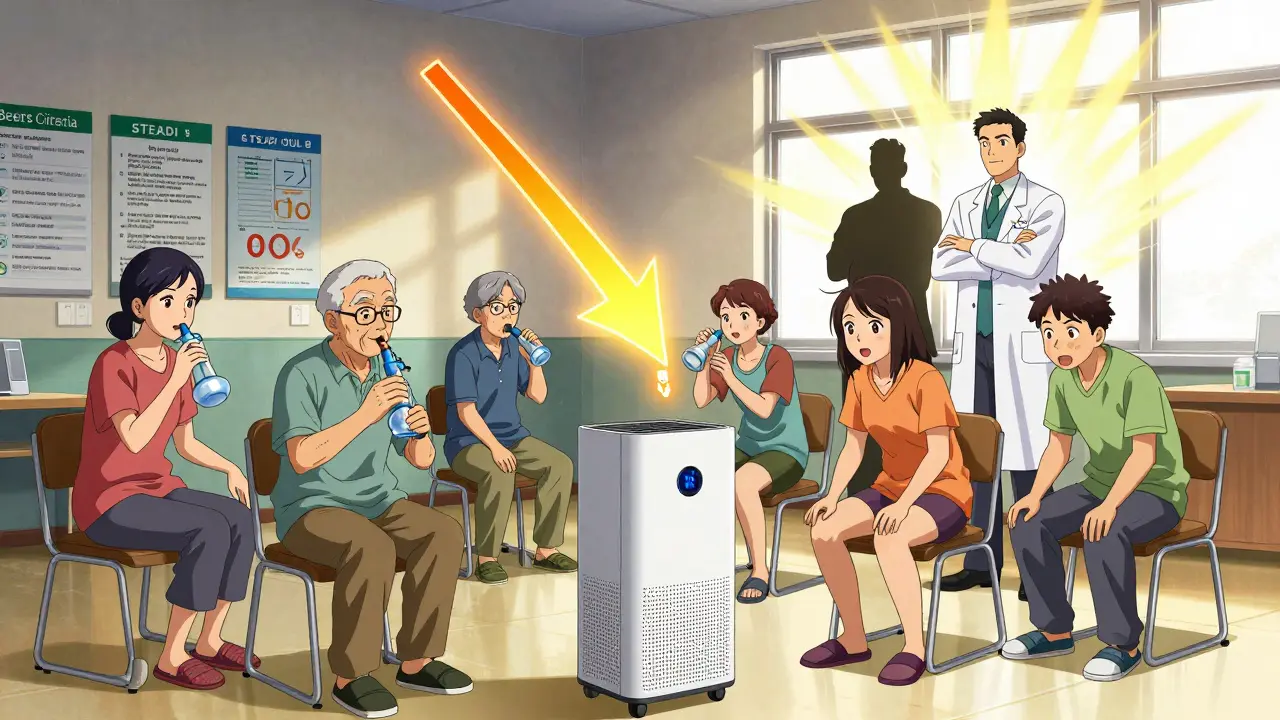
The CDC’s STEADI program calls this the “3S” approach: Stop, Switch, Reduce. It’s simple. It’s proven. And it works.
Non-Medication Alternatives That Actually Work
You don’t need a pill to manage allergies or sleep better. There are safer, more effective ways.
- Nasal saline rinses reduce allergy symptoms by 35-40%. Use a neti pot or squeeze bottle with sterile salt water every morning.
- Allergen-proof bedding cuts dust mite exposure by 83%. Buy pillow and mattress covers made of tightly woven fabric.
- HEPA air purifiers remove 99.97% of airborne allergens. Place one in the bedroom. It’s cheaper than years of allergy meds.
- Sleep hygiene is the best fix for insomnia. No caffeine after noon. No screens an hour before bed. Keep your room cool and dark. Stick to the same bedtime every night.
These aren’t “alternative” ideas. They’re evidence-backed, doctor-recommended, and zero-risk. And they work better than any antihistamine ever could.
What Your Pharmacist Can Do for You
Most people don’t realize pharmacists can help with medication safety. Ask for a “brown bag review.” Bring all your pills, supplements, and OTC products to your pharmacy. The pharmacist will check for dangerous combinations, outdated meds, and high-risk drugs like diphenhydramine.
Studies show pharmacist-led reviews reduce fall risk by 26% in older adults. That’s not a small benefit. That’s life-changing. And it takes 20 minutes. No appointment needed. Just walk in.
Pharmacists are trained to spot these risks. They see what doctors miss. Don’t wait for your doctor to bring it up. Take the initiative. Bring your bag.
Environmental Changes That Prevent Falls
Even if you stop the meds, your home might still be dangerous. Falls don’t happen because of one thing-they happen because of many small risks adding up.
- Install grab bars in the bathroom. Near the toilet and in the shower. They reduce fall risk by 28%.
- Improve lighting. Add nightlights in hallways and bathrooms. Use bright bulbs. Shadows and dim corners are fall traps.
- Remove tripping hazards. Get rid of loose rugs. Tuck away cords. Keep floors clear. A single rug causes more falls than all the antihistamines combined.
- Wear proper shoes. No slippers. No socks on hardwood. Wear sturdy, non-slip shoes-even indoors.
These changes cost less than $200. They take a weekend. And they save lives.
What’s Changing in 2026
There’s good news. The system is starting to catch up.
Since 2024, Medicare’s Annual Wellness Visit now requires doctors to review all high-risk medications-including antihistamines-as part of fall risk screening. That means you can’t avoid the conversation anymore.
The American Geriatrics Society updated its Beers Criteria in 2025 to be even stricter. The FDA is now pushing for stronger OTC labels. And two new antihistamines are in clinical trials-designed specifically for older adults with almost no brain penetration. Early results show 89% less drowsiness than diphenhydramine.
But waiting for new drugs isn’t the answer. The tools we have now-switching meds, cleaning up the home, talking to your pharmacist-can stop falls today. You don’t need to wait for the future to protect yourself.
Final Thought: Safety Isn’t About Pills
Older adults don’t need more medication. They need fewer dangerous ones. They need better sleep, cleaner air, safer homes, and more support-not more pills that make them dizzy.
If you or someone you love is taking Benadryl for sleep or allergies, stop. Don’t wait for a fall. Don’t wait for a doctor to mention it. Do it now. Switch to fexofenadine. Use a neti pot. Install a grab bar. Call your pharmacist. These steps aren’t hard. They’re just overlooked.
Every year, 32,000 older adults die from falls. Many of those deaths could have been prevented. With one simple change: swapping a dangerous pill for a safe one.
Is diphenhydramine safe for older adults?
No. Diphenhydramine is not safe for older adults. It significantly increases the risk of falls, confusion, delirium, and fractures. The American Geriatric Society explicitly advises against its use in people over 65. Even small doses can cause prolonged drowsiness and impaired balance.
What’s the safest antihistamine for seniors?
Fexofenadine (Allegra) is the safest. It causes almost no drowsiness and has no anticholinergic effects. Loratadine (Claritin) is also very safe. Cetirizine (Zyrtec) is acceptable for some, but it causes mild drowsiness in about 14% of older adults, so use it with caution.
Can I stop taking diphenhydramine cold turkey?
Yes, if you’re using it for allergies. But if you’ve been taking it for sleep, stopping suddenly may cause temporary rebound insomnia. In that case, replace it with better sleep habits first: fixed bedtime, no screens before bed, cool dark room. Then stop the pill. Don’t switch to another sedative.
How long does diphenhydramine stay in an older person’s system?
In healthy adults, it lasts about 8.5 hours. In older adults, it can last 13.5 hours or longer. Peak drowsiness hits 1-3 hours after taking it, but the effects can linger for 6-8 hours or more, especially if taken daily.
Do second-generation antihistamines have any risks?
They’re much safer, but not zero-risk. Cetirizine can cause mild drowsiness in 14% of older adults. Always start with the lowest dose. If you feel lightheaded or unsteady after taking any antihistamine, stop and talk to your doctor.
Can I use allergy shots instead of pills?
Yes. Allergy immunotherapy (shots or tablets) is a long-term solution that reduces the need for daily antihistamines. It’s especially helpful for seniors with chronic allergies. Talk to an allergist-this can eliminate the need for pills entirely.
Should I ask my doctor to review all my medications?
Absolutely. Everyone over 65 should have a full medication review at least once a year. Bring all your pills, vitamins, and OTC meds to the appointment. Ask: “Are any of these linked to falls or dizziness?” This simple step can prevent serious injury.



JUNE OHM
January 2, 2026 AT 16:11Vincent Sunio
January 3, 2026 AT 06:29Kerry Howarth
January 3, 2026 AT 13:33Stop. Switch. Reduce.
Simple. Clear. Life-saving.
Angela Goree
January 4, 2026 AT 01:16Joy F
January 5, 2026 AT 21:57Philip Leth
January 7, 2026 AT 18:17Haley Parizo
January 9, 2026 AT 05:20Ian Detrick
January 10, 2026 AT 14:03Tiffany Channell
January 12, 2026 AT 13:24Shanahan Crowell
January 12, 2026 AT 17:52