Why Clear Medication Communication Matters
Half of all people taking medication for chronic conditions don’t take it as prescribed. That’s not because they’re lazy or forgetful-it’s often because they simply don’t understand what they’re supposed to do, why it matters, or what to expect. A 2020 study in the Annals of Internal Medicine found that poor communication around medications costs the U.S. healthcare system over $300 billion a year in avoidable hospital visits, emergency care, and worsening conditions. The fix isn’t more pills or higher doses-it’s clearer conversations.
When a doctor says, “Take this twice a day,” that’s not enough. Patients hear it, nod, and leave. But what does “twice a day” mean? Before breakfast and dinner? With food or on an empty stomach? Will they feel better in a day or a week? What if they feel dizzy? Should they stop? Without answers to these questions, patients guess-and guessing with medication is dangerous.
What Patients Really Need to Know
Patients don’t need a pharmacology lecture. They need to know four things:
- Why they’re taking this medication-what problem it’s meant to fix
- How to take it-exact timing, with or without food, what to avoid
- What to expect-when they’ll start to feel better, what side effects are normal, when to worry
- What to do if things go wrong-when to call, when to stop, when to show up at the clinic
One 68-year-old woman with high blood pressure told her provider she stopped her pill because “it made me tired.” Her provider assumed she was noncompliant. But when they asked what she meant by “tired,” she said she couldn’t play with her grandkids anymore. Turns out, the medication was lowering her blood pressure too much. That conversation never happened because the provider never asked. The fix wasn’t a new drug-it was a better question.
The Teach-Back Method: The Gold Standard
The most proven way to make sure patients understand is called the Teach-Back method. It’s simple: after explaining something, ask the patient to explain it back in their own words. Not “Do you understand?”-that’s a yes/no trap. Instead, say: “To make sure I explained this right, can you tell me how you’ll take this pill?”
Studies show this boosts adherence by 23%. The Joint Commission International calls it non-negotiable for high-risk meds like blood thinners, insulin, or heart medications. A 2021 study at UCSF found that when providers used Teach-Back consistently, 30-day medication adherence jumped from 62% to 84% in patients with diabetes and heart failure.
It’s not about testing patients. It’s about testing your explanation. If they can’t repeat it clearly, you didn’t communicate well enough. That’s not their fault-it’s yours. And it’s fixable.
Plain Language, Not Medical Jargon
Never say “Take PO BID.” That means “by mouth, twice a day”-but 80 million American adults have trouble reading even basic health materials, according to the AHRQ. Saying “Take one pill when you wake up and one when you go to bed” is clear. Saying “This reduces your risk by 20%” sounds impressive-but if their baseline risk was 10%, that means it goes down to 8%. That’s not a miracle. It’s a small but real benefit. Say it that way: “Out of 100 people like you, 10 would have a heart attack in 10 years without this pill. With it, only 8 would.”
Use analogies. “This medicine works like a sponge soaking up extra fluid in your legs.” “The antibiotic kills the bad bacteria like a mop cleaning up a spill.” Avoid words like “compliance,” “adherence,” or “therapeutic.” Say “take as directed” instead of “follow the regimen.”
Timing, Timing, Timing
Patients want to know: When will I feel something? Too many stop meds because they expect instant results. A blood pressure pill might take 2-3 weeks to show full effect. An antidepressant can take 4-6 weeks. If you don’t say that upfront, they’ll assume it’s not working and quit.
Be specific: “Most people notice less swelling in their ankles after about 10 days.” “The pain might get worse before it gets better-this happens in the first week for about 1 in 5 people.”
Also, be honest about what won’t change. “This won’t cure your arthritis, but it should let you walk farther without pain.” Setting realistic expectations prevents disappointment and builds trust.
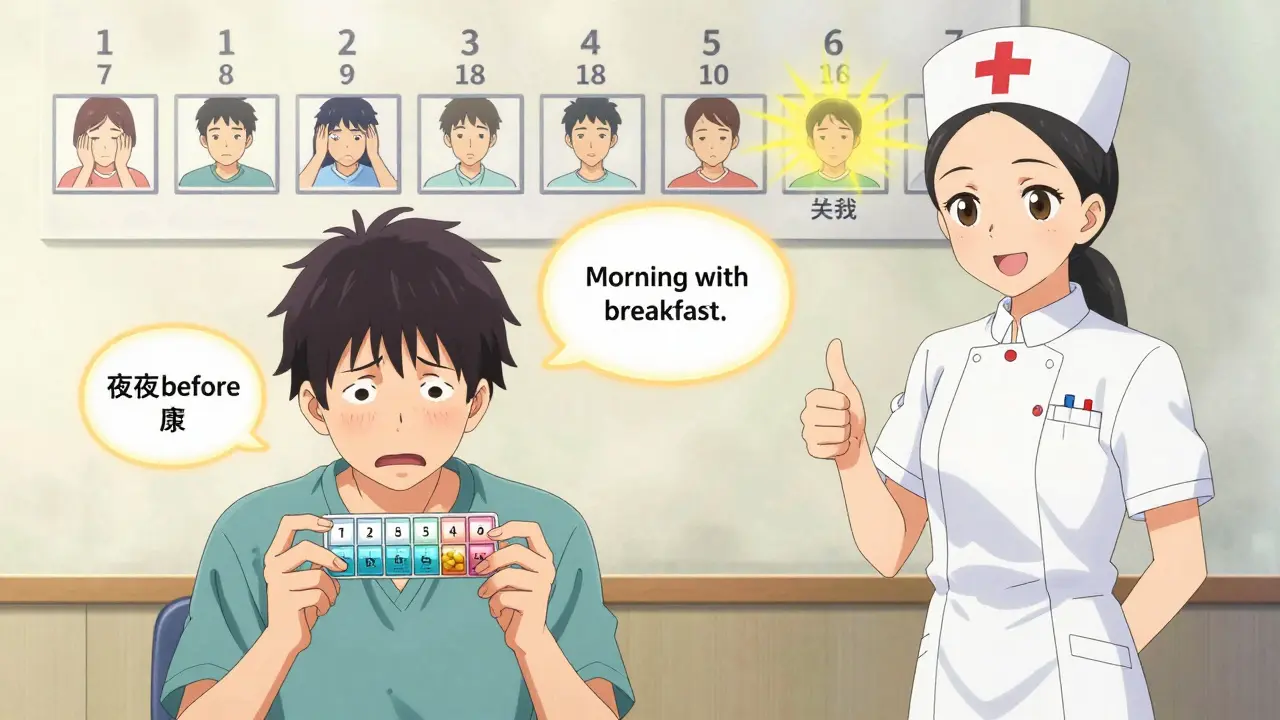
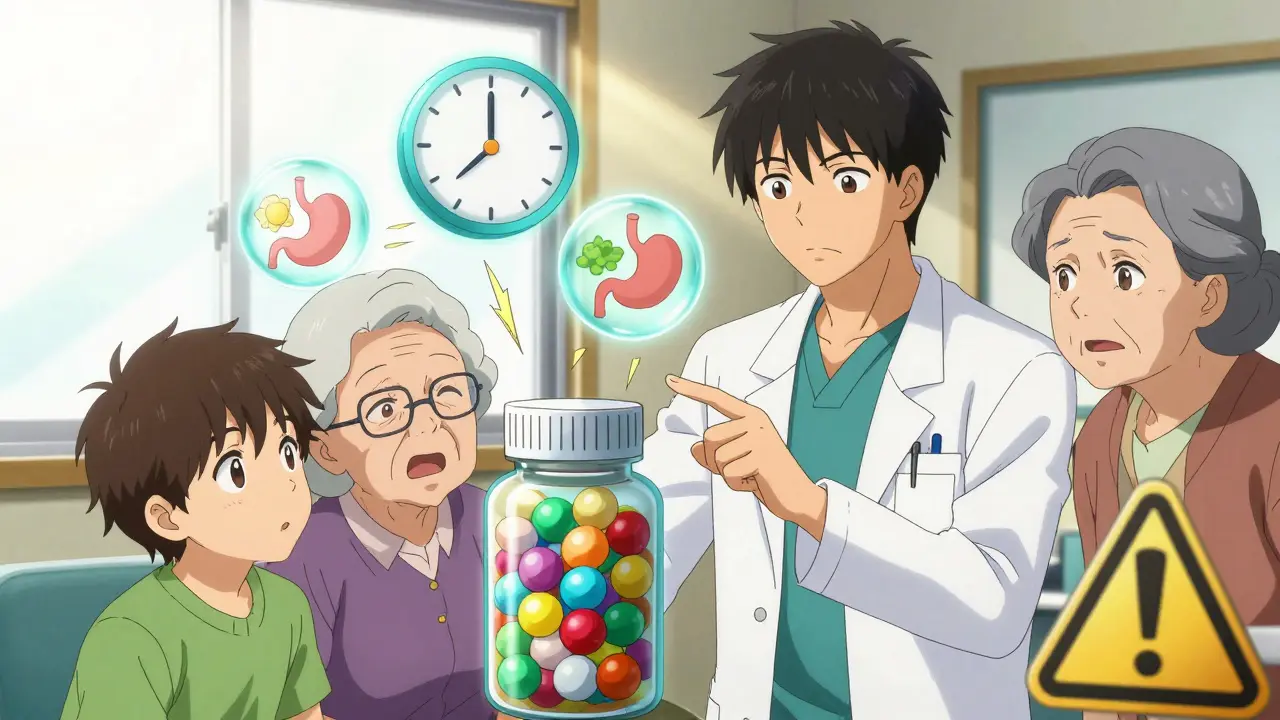
Use Visuals and Tools
A picture is worth a thousand words-especially when it comes to pills. Show the patient the actual pill bottle. Point to the label. Use a pill organizer with the days of the week. Draw a simple timeline: “Day 1-3: Might feel a little dizzy. Day 4-10: You’ll start to sleep better. Day 14: You should feel more energy.”
Many clinics now use printed handouts with icons: a clock for timing, a stomach for food instructions, a warning sign for side effects. Even better-have the patient point to the pill in the bottle and say when they’ll take it. If they can’t, you haven’t finished the conversation.
What to Avoid
Here’s what doesn’t work:
- “Take as directed.” - Too vague. What does that mean?
- “It’s important you take this.” - Sounds like guilt, not education.
- “This is standard.” - Patients don’t care what’s standard. They care what’s right for them.
- Speed-talking. Most providers speak at 180+ words per minute. Patients can only process 130-150. Slow down. Pause. Let them ask.
- Not asking about concerns. “Any questions?” is a trap. Most patients won’t say, “I’m scared this will make me gain weight.” But “What worries you most about taking this?” opens the door.

How to Fit This Into a Busy Day
Doctors have 15.7 minutes per visit, on average. That’s not much. But you don’t need more time-you need better structure.
Try this 5-step routine:
- Ask first: “What has your doctor told you about this medication?” This tells you what they already think-and what’s wrong.
- Explain simply: Use plain language. One or two key points only. “This lowers your blood pressure so your heart doesn’t have to work as hard.”
- Give a timeframe: “You’ll start to feel better in 2-3 weeks.”
- Show the pill: Point to the bottle. Show the schedule.
- Teach-back: “Can you tell me how and when you’ll take this?”
This takes 2-3 minutes. It’s not extra time-it’s smarter time.
Some clinics now schedule 10-minute “medication check-ins” with pharmacists for patients on 5 or more drugs. Those visits cut hospitalizations by 22%. If your clinic doesn’t have one, ask for it.
What Happens When You Do This Right
Patients who feel they truly understand their meds are more likely to:
- Take them as prescribed
- Ask questions when something feels off
- Keep follow-up appointments
- Report side effects early
- Trust you
Press Ganey’s 2023 survey found that 78% of patients who rated their understanding as “excellent” said their provider used examples they could relate to and checked that they understood. One patient wrote: “My doctor drew a picture of how the pill worked in my body. I finally got it.” Another: “The nurse had me show how I’d use my inhaler before I left. That’s the first time anyone ever did that.”
The Future Is Here
Technology is helping. EHRs now have built-in templates to document medication goals. Text reminders say: “Remember, dizziness the first week is normal-don’t stop.” AI tools are being tested to listen to conversations and flag when Teach-Back was skipped. Starting in 2025, Medicare will reward doctors who prove patients understand their meds-with up to a 20% bonus.
This isn’t about checking a box. It’s about saving lives. Every time you make a medication conversation clear, you’re not just giving a pill-you’re giving control. And that’s the most powerful medicine of all.
What is the Teach-Back method and why is it so effective?
The Teach-Back method is when a healthcare provider explains something to a patient and then asks the patient to repeat it back in their own words. It’s effective because it doesn’t assume understanding-it tests it. Studies show it increases medication adherence by 23%. It catches misunderstandings before patients leave the office. For example, if a patient says they’ll take a pill “when I feel sick,” but the provider meant “every morning,” that mistake is caught and fixed right away. It’s not about testing the patient-it’s about improving the provider’s communication.
How do I explain medication side effects without scaring patients?
Use numbers and context. Instead of saying, “One in five people get nausea,” say, “About 1 out of 5 people feel a little queasy the first week, but it usually goes away. If it lasts longer than a week or gets worse, call us.” Focus on what’s normal versus what’s dangerous. Most side effects are mild and temporary. Let patients know what’s expected so they don’t panic and stop the medicine. Also, ask them what worries them most-that often reveals their real fear.
What should I do if a patient says they don’t want to take a medication?
Don’t argue. Ask why. “What’s making you hesitate?” might reveal they’re afraid of weight gain, think it’s too expensive, or heard a bad story from a friend. Listen first. Then, connect the medicine to their goals. If they want to play with their grandkids, explain how this pill helps them have more energy. Offer alternatives if possible. Sometimes, a different pill, a lower dose, or a different schedule works better. The goal isn’t to get them to say yes-it’s to help them make a choice that fits their life.
Can I use family members to help with medication communication?
Yes-especially for older adults or those with memory issues. Ask if they’d like a family member to join the conversation. Make sure the person helping understands the schedule, side effects, and warning signs. Have them repeat the instructions back too. Many patients rely on family to manage pills, so including them isn’t optional-it’s essential. Just make sure the patient still understands and agrees. Their consent matters most.
How do I know if I’m communicating clearly enough?
If the patient can explain the purpose, schedule, and what to expect without you helping, you’re clear. If they say “I’ll take it when I remember,” you’re not. If they can’t name one side effect or when to call you, you’re not. Use the Teach-Back method every time. If you’re unsure, ask: “What’s one thing you’ll tell your spouse about this pill?” Their answer tells you everything.





Daz Leonheart
February 2, 2026 AT 15:28